Better, higher, lower, faster: increasingly rapid clinical decision making using high-sensitivity cardiac troponin assays
Since the introduction of the high-sensitivity cardiac troponin assays, the diagnosis of acute myocardial infarction without ECG abnormalities has undergone a transformation. This is clearly illustrated by a recent research paper by Mueller-Hennessen and colleagues, which focused on the rule-in of patients for the diagnosis of acute myocardial infarction without consecutive measurements (1). At first sight, the scope of this study may seem to be at odds with the limited specificity of (small) cardiac troponin elevations (2,3), and the required rise or fall in cardiac troponin concentrations of most (traditional) diagnostic guidelines (4,5). However, it perfectly represents the trend of increasingly rapid clinical decision making in patients with suspected acute myocardial infarction. In addition, the study provides important evidence for the immediate rule in of patients with chest pain and high troponin values. In this Editorial, we reflect on the rapid rule-in and rule-out of acute myocardial infarction according to the recently introduced 0-/1-hour algorithm, its performance, and future challenges.
Make it better—diagnosis of acute myocardial infarction in the high-sensitivity assay era
Before the introduction of high-sensitivity assays, time-intervals of six to nine hours were required to detect a significant rise or fall in cardiac troponin levels, and thus to provide patients with a final diagnosis (6). Due to the introduction of increasingly sensitive assays, laboratories became able to detect and report cardiac troponin concentrations in the lower range, and to accurately distinguish small changes in serially measured cardiac troponin levels (7). This enabled further refinement in clinical decision making. First, it triggered the exploration of increasingly shorter time intervals between consecutive measurements and the development of new, more rapid diagnostic algorithms. Second, as a consequence of the improved assays and consecutive ability to quantify cardiac troponin concentrations in the lower range, it renewed the interest in diagnostics based on a single cardiac troponin measurement at presentation (8).
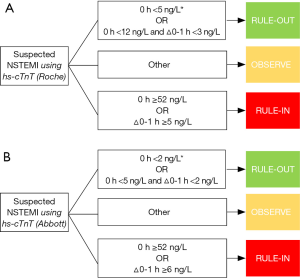
These evolutions are clearly evident in the international guidelines: In 2011, the fastest diagnostic algorithm in the guidelines of the European Society of Cardiology (ESC) contained a 3-hour interval between the first blood draw at presentation and the second, consecutive one. Four years later, in 2015, the updated version of these guidelines contained an even faster algorithm in which the time-interval was reduced to one hour, and included cut-off values for rule-in and rule-out after a single blood draw at presentation (5,9) (Figure 1).
Include the higher—time is muscle
The rapid identification of patients with acute myocardial infarction offers major advantages, like fast transfer to a cardiology unit for monitoring and accelerated initiation of interventions (1,10). The 0-/1-hour algorithm of the 2015 ESC guidelines includes two pathways for rapid rule-in: (I) direct rule-in if the cardiac troponin concentration is above an assay specific cut-off value [52 ng/L for both hs-cTnT (Roche Cobas) and hs-cTnI (Abbott Architect)], and (II) rule-in after a consecutive one-hour measurement after if the absolute change between the two serial measurements is above an assay specific cut-off value [5 ng/L for hs-cTnT (Roche Cobas)) and 6 ng/L for hs-cTnI (Abbott Architect)] (5) (Figure 1).
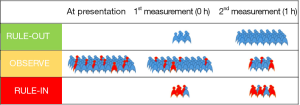
Several studies showed that accurate rule-in of myocardial infarction is feasible with the 0-/1-hour algorithm (positive predictive value 74–78%) (11-14). As a result of the use of the 0-/1-hour algorithm, approximately 70% of the patients with acute myocardial infarction can be ruled-in following a second cardiac troponin measurement after one hour (Figure 2). However, even earlier rule-out, after a single blood draw at presentation, seems to be feasible in a substantial number of patients. Recently, Mueller-Hennessen and colleagues examined the additional value of kinetic changes in patients presenting with highly abnormal cardiac troponin T concentrations at presentation. They demonstrated that serial cardiac troponin T measurements do not add incremental diagnostic value in patients with initial cardiac troponin concentrations >60 ng/L. In clinical practice this would mean that monitoring of kinetic changes for rule-in seems not to be required for approximately 7% of patients presenting with chest pain (22% of subjects with an actual acute myocardial infarction) (1). Despite the slight differences in cut-off value and population (the study by Mueller-Hennessen included both patients with or without ST-elevations on ECG), the results of this study are in support of the current guidelines that facilitate very early rule-in.
Exclude the lower—prevent unnecessary waiting
Only a minority of subjects, approximately 15–20%, that is evaluated at the emergency department because of chest pain does have an actual acute myocardial infarction (1,13,17). Since the majority of patients do not have an acute myocardial infarction, the rapid rule-out of these patients is of profound importance; it can overcome prolonged patient anxiety, unnecessary resource use and overcrowding in the emergency department (7,18-23). However, whereas a missed diagnosis of acute coronary syndrome is clearly associated with higher mortality, early rule-out is a delicate process that requires an extremely low miss-rate. This is reflected in a high sensitivity and high negative predictive value of the optimal cut-off values (24).
The 0-/1-hour algorithm of the 2015 ESC guidelines contains two approaches for the rapid rule-out of patients: (I) Direct rule-out at presentation if the chest pain is present for more than three hours and the cardiac troponin concentration is below an assay-specific cut-off value [5 ng/L for hs-cTnT (Roche Cobas) or 2 ng/L for hs-cTnI (Abbott Architect)], and (II) rule-out after a consecutive measurement after one hour if both the initial cardiac troponin concentration and the absolute change between the two serial measurements are below assay-specific cut-off values [respectively 12 and 3 ng/L for hs-cTnT (Roche Cobas) or 5 and 2 ng/L for hs-cTnI (Abbott Architect)] (5) (Figure 1).
Using this algorithm, approximately 75% of all subjects without acute myocardial infarction can be ruled-out after one hour; a minority after a single blood draw at presentation and the majority following a consecutive measurement (Figure 2) (11,13,14). The negative predictive value of this approach was excellent (99.9–100%) in the original derivation cohort, but recently turned out to be slightly lower for troponin T (99.1%) in an external validation cohort (11).
The fact that a significant number of subjects still have to wait an additional hour on the emergency department before they can be ruled-out triggered the exploration of alternative rule-out strategies. During the last couple of years, a substantial number of articles have been published that explored the possibilities of rule-out with a single blood draw at presentation. The use of higher cut-off values, like 5 ng/L for cardiac troponin T or 6 ng/L for cardiac troponin I, and the application of these values on both early and late presenters in these studies increased the number of direct rule-outs, but was often on the expense of the negative predictive value (15,25-29).
Do it faster—future strategies
Using the 0-hour/1-hour diagnostic algorithm, 70–75% of all patients can be ruled-in or rule-out after a second measurement at one hour (11,16). However, the quest to better and more efficient healthcare, keeps challenging us to develop even more rapid and safe diagnostic algorithms. There are several possible strategies to address this challenge.
A first strategy for the further reduction of the mean time from presentation to diagnosis, focuses on the 25–30% of subjects that remain in the observational zone after the second cardiac troponin measurement. The early implementation of additional biomarkers or modalities, like imaging or functional testing, in the diagnostic pathway needs further exploration in this particular group of patients (16).
Whereas a second measurement is indicated in a substantial number of patients, a second strategy involves the optimization of the cut-off values at presentation. However, some considerations on this approach merit attention. First, and most important: What is the price—the amount of false discharges or false initiations of treatments-, we are willing to pay for an overall shorter mean time from presentation to diagnosis. In order to obtain maximum rule-in or rule-out with a high predictive value, the setting of cut-off values in cohort studies is often strongly driven by outliers (30). With the current approach, using only cardiac troponin T or cardiac troponin I, we seem to approach the limit of what is safely feasible. Second, considering rule-out, we should be aware of the fact that some individuals with acute myocardial infarction, but without persistently elevated cardiac troponin levels who present early after chest pain onset may be missed when we apply higher cut-off values for direct rule-out or when we apply cut-off values to all patients, early and late presenters (15).
In addition to the considerations above, a third strategy involves the further exploration of combinations of cardiac troponin concentrations with imaging and/or other (cardiac) biomarkers (25).
Other approaches to shorten the mean time from presentation to diagnosis include shorter turnaround times in the emergency department and the laboratory (e.g., by the use of point-of-care-assays), and shorter time-intervals between consecutive measurements. However, it is not yet clear whether these approaches are achievable, profitable and safe for use in clinical practice.
Future research in the field of increasingly rapid diagnostics for acute myocardial infarction seems to be inevitable: Our work is never over (31).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Jingyu Guo (State Key Laboratory of Pathogen and Biosecurity, Beijing Institute of Microbiology and Epidemiology, Beijing, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jlpm.2017.04.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mueller-Hennessen M, Mueller C, Giannitsis E, et al. Serial Sampling of High-Sensitivity Cardiac Troponin T May Not Be Required for Prediction of Acute Myocardial Infarction Diagnosis in Chest Pain Patients with Highly Abnormal Concentrations at Presentation. Clin Chem 2017;63:542-51. [Crossref] [PubMed]
- Giannitsis E, Katus HA. Cardiac troponin level elevations not related to acute coronary syndromes. Nat Rev Cardiol 2013;10:623-34. [Crossref] [PubMed]
- Boeddinghaus J, Reichlin T, Nestelberger T, et al. Early diagnosis of acute myocardial infarction in patients with mild elevations of cardiac troponin. Clin Res Cardiol 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;130:2354-94. [Crossref] [PubMed]
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267-315. [Crossref] [PubMed]
- Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Eur Heart J 2007;28:2525-38. [Crossref] [PubMed]
- Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 2009;361:858-67. [Crossref] [PubMed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J 2012;33:2551-67. [Crossref] [PubMed]
- Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2011;32:2999-3054. [Crossref] [PubMed]
- Mehta SR, Granger CB, Boden WE, et al. Early versus delayed invasive intervention in acute coronary syndromes. N Engl J Med 2009;360:2165-75. [Crossref] [PubMed]
- Mueller C, Giannitsis E, Christ M, et al. Multicenter Evaluation of a 0-Hour/1-Hour Algorithm in the Diagnosis of Myocardial Infarction With High-Sensitivity Cardiac Troponin T. Ann Emerg Med 2016;68:76-87.e4. [Crossref] [PubMed]
- Rubini Gimenez M, Twerenbold R, Jaeger C, et al. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. Am J Med 2015;128:861-870.e4. [Crossref] [PubMed]
- Reichlin T, Twerenbold R, Wildi K, et al. Prospective validation of a 1-hour algorithm to rule-out and rule-in acute myocardial infarction using a high-sensitivity cardiac troponin T assay. CMAJ 2015;187:E243-52. [Crossref] [PubMed]
- Jaeger C, Wildi K, Twerenbold R, et al. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. Am Heart J 2016;171:92-102.e1-5.
- Boeddinghaus J, Nestelberger T, Twerenbold R, et al. Direct Comparison of Four Very Early Rule-Out Strategies for Acute Myocardial Infarction Using High-Sensitivity Cardiac Troponin I. Circulation 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Nestelberger T, Wildi K, Boeddinghaus J, et al. Characterization of the observe zone of the ESC 2015 high-sensitivity cardiac troponin 0h/1h-algorithm for the early diagnosis of acute myocardial infarction. Int J Cardiol 2016;207:238-45. [Crossref] [PubMed]
- Meller B, Cullen L, Parsonage WA, et al. Accelerated diagnostic protocol using high-sensitivity cardiac troponin T in acute chest pain patients. Int J Cardiol 2015;184:208-15. [Crossref] [PubMed]
- Reiter M, Twerenbold R, Reichlin T, et al. Early diagnosis of acute myocardial infarction in patients with pre-existing coronary artery disease using more sensitive cardiac troponin assays. Eur Heart J 2012;33:988-97. [Crossref] [PubMed]
- Thygesen K, Mair J, Giannitsis E, et al. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J 2012;33:2252-7. [Crossref] [PubMed]
- Raskovalova T, Twerenbold R, Collinson PO, et al. Diagnostic accuracy of combined cardiac troponin and copeptin assessment for early rule-out of myocardial infarction: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care 2014;3:18-27. [Crossref] [PubMed]
- Lipinski MJ, Baker NC, Escarcega RO, et al. Comparison of conventional and high-sensitivity troponin in patients with chest pain: a collaborative meta-analysis. Am Heart J 2015;169:6-16.e6. [Crossref] [PubMed]
- Mockel M, Searle J, Hamm C, et al. Early discharge using single cardiac troponin and copeptin testing in patients with suspected acute coronary syndrome (ACS): a randomized, controlled clinical process study. Eur Heart J 2015;36:369-76. [Crossref] [PubMed]
- Collinson P, Gaze D, Goodacre S. Comparison of contemporary troponin assays with the novel biomarkers, heart fatty acid binding protein and copeptin, for the early confirmation or exclusion of myocardial infarction in patients presenting to the emergency department with chest pain. Heart 2014;100:140-5. [Crossref] [PubMed]
- Scheuermeyer FX, Innes G, Grafstein E, et al. Safety and efficiency of a chest pain diagnostic algorithm with selective outpatient stress testing for emergency department patients with potential ischemic chest pain. Ann Emerg Med 2012;59:256-264.e3. [Crossref] [PubMed]
- Shortt C, Ma J, Clayton N, et al. Rule-In and Rule-Out of Myocardial Infarction Using Cardiac Troponin and Glycemic Biomarkers in Patients with Symptoms Suggestive of Acute Coronary Syndrome. Clin Chem 2017;63:403-14. [Crossref] [PubMed]
- Sandoval Y, Smith SW, Shah AS, et al. Rapid Rule-Out of Acute Myocardial Injury Using a Single High-Sensitivity Cardiac Troponin I Measurement. Clin Chem 2017;63:369-76. [Crossref] [PubMed]
- Neumann JT, Sorensen NA, Ojeda F, et al. Immediate Rule-Out of Acute Myocardial Infarction Using Electrocardiogram and Baseline High-Sensitivity Troponin I. Clin Chem 2017;63:394-402. [Crossref] [PubMed]
- Body R, Burrows G, Carley S, et al. High-sensitivity cardiac troponin t concentrations below the limit of detection to exclude acute myocardial infarction: a prospective evaluation. Clin Chem 2015;61:983-9. [Crossref] [PubMed]
- Shah AS, Anand A, Sandoval Y, et al. High-sensitivity cardiac troponin I at presentation in patients with suspected acute coronary syndrome: a cohort study. Lancet 2015;386:2481-8. [Crossref] [PubMed]
- Pickering JW, Than MP. The small number problem in diagnostic algorithms and why we need to bootstrap. Clin Biochem 2017; [Epub ahead of print]. [Crossref] [PubMed]
- DaftPunk. Harder, better, faster, stronger [single]. London, United Kingdom: Virgin Records, 2001.
Cite this article as: van der Linden N, Streng AS, Wodzig WKWH, Bekers O, Meex SJR. Better, higher, lower, faster: increasingly rapid clinical decision making using high-sensitivity cardiac troponin assays. J Lab Precis Med 2017;1:14.