Serum bilirubin has an important role in multiple clinical applications
Bilirubin has been deemed to be a natural end-product of heme metabolism in the body and has a neurotoxic effect in infants (1). However, accumulating data have demonstrated that serum bilirubin has anti-oxidative, anti-inflammatory and immunosuppressive functions in various diseases (2). Indeed, serum bilirubin has been found to be a predictor in some oxidative stress-mediated diseases, including atherosclerosis, rheumatism and neuropsychiatric disorders (3). Further, numerous studies have provided evidence that mildly elevated serum bilirubin concentrations are associated with better prognosis in cardiovascular, autoimmune and oncologic diseases (4). Serum bilirubin levels have been reported to be related to type 2 diabetes mellitus (T2DM) and its complications (5). The relationships between serum bilirubin concentrations and essential trace elements status have also been revealed in an adult population since serum bilirubin maintains strong anti-inflammatory and anti-oxidative features even in general population (6). In fact, oxidative stress, inflammation, and immune response contribute to the pathology and physiology of clinical diseases and serve as triggers in these diseases (7). Therefore, it is reasonable to speculate that serum bilirubin is a promising biomarker to assess severity and prognosis of certain diseases in clinical laboratory medicine. In this article, we summarized the published studies in regard to levels of serum bilirubin and its relation with severity and prognosis of clinical diseases and disorders, and its clinical implications are reviewed.
Serum bilirubin and cardiovascular diseases (CVD)
Bilirubin is a considered as a non-traditional risk factor in patients with CVD owing to its anti-oxidative and anti-inflammatory actions. A relationship between serum bilirubin and CVD was first reported by Schwertner et al. (8) in 1994. Their study demonstrated that in adult males serum bilirubin is an independent risk factor for asymptomatic and angiographically proven coronary artery disease (CAD) even after adjusting for age, total cholesterol, smoking and systolic blood pressure (SBP). From a prospectively collected data on 7,658 middle-aged British males, followed for 11.6 years, Breimer et al. (9) found a negative association between serum bilirubin and ischemic heart disease. Since then, multiple studies have suggested that serum bilirubin plays an important role in the development of CVD.
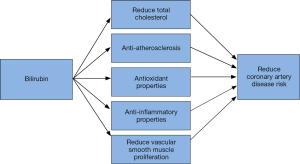
Although the main mechanism related to an interaction of serum bilirubin and CVD is obscure, various theories have been proposed as shown in Figure 1. Hyperbilirubinemia reduces circulating plasma lipids such as cholesterol, triacylglycerols and low-density lipoprotein (LDL) cholesterol (10). Patients with higher bilirubin were found to have a lower risk of CVD events since its potential protective role against atherosclerosis process (11). Bilirubin could protect against atherosclerosis process due to its antioxidant and anti-inflammatory properties as well as inhibition of vascular smooth muscle cell proliferation (12). Ko et al. (13) reported an inverse relationship between the levels of serum bilirubin and other known CVD risk factors such as smoking, obesity, SBP, glycated hemoglobin, triglycerides and LDL levels. de Sauvage Nolting et al. (14) found that in patients with familial hypertriglyceridemia, baseline serum bilirubin concentration is inversely associated with the presence of CVD even after adjusting for age, sex, HTN, and HDL cholesterol levels. In a cross-sectional cohort of healthy Japanese adults, it was found that high bilirubin levels are associated with less CVD and stroke prevalence in males and less prevalence of stroke in females (15) after adjusting common risk factors. Lower serum bilirubin has been found to be associated with all-cause mortality and cardiovascular mortality in patient with kidney dysfunction (16). Lin et al. (17) discovered that serum bilirubin is negatively related to SYNTAX score in patients with stable CAD, and can predict future cardiovascular events such as non-fatal myocardial infarction, target vessel revascularization, stroke and death. A large scale population studies have found an inverse relationship between serum bilirubin concentration and incidence of hypertension (18). Ex vivo studies on rats’ heart have shown that pre- and post-treatment with bilirubin ditaurate provide significant cardioprotection, with a reduction in infarct size and oxidative damage (19). From the above evidences, it is clear that mildly elevated bilirubin level has cardioprotective effects and this relation should be further studied in animal and human experimental trials.
Serum bilirubin and autoimmune disorders (AIDs)
AIDs are a group of disorders in which the immune system “attacks” itself due to exaggerated recognition and response to antigens, causing tissue damage and chronic inflammation. Continued oxidative stress, chronic inflammation, and immune response play a key role in the pathogenesis of AIDs. Because of its direct anti-oxidative, anti-inflammatory and immunomodulatory properties, mildly elevated bilirubin has been demonstrated to be beneficial in patients with AIDs (20). In a sample of 8,147 individuals in NHANES (National Health and Nutrition Examination Survey) study from 2003–2006, the prevalence of rheumatoid arthritis was inversely related to total serum bilirubin level (OR: 0.679; 95% CI 0.533–0.865) (21). In a study, it was found that serum bilirubin levels are significantly lower in newly diagnosed polymyositis patients when compared to healthy controls, and bilirubin levels negatively correlate to ESR, CK and LDH in patients with polymyositis (22). Moreover, serum bilirubin was found to be inversely correlated with disease activity and extent in patients with systemic lupus erythematosus (SLE) (20). Furthermore, each 1 µmol/L decrease in serum bilirubin is associated with a 37% increase in the odds for a positive SLE status (OR: 1.37; 95% CI 1.28–1.47, P<0.00001) (23). Another study in SLE patients showed significantly decreased total, indirect and direct bilirubin levels but only lower direct bilirubin levels show an independent association with renal involvement due to lupus (24). It was proposed that conjugated bilirubin can be filtered by glomeruli which could exert local (renal) anti-oxidative and anti-inflammatory effects while unconjugated bilirubin cannot (25). Serum bilirubin levels were found to be significantly lower (P<0.001) in patients with multiple sclerosis (MS) when compared to healthy adults. However, authors also discovered that patients with longer duration of MS >2 years, lower disability score and inactive disease on MRI had lower concentration of bilirubin. The authors could not explain if it was due to the primary deficit or increased consumption of bilirubin by free radicals. Similar findings were also observed in patients with myasthenia gravis, Takayasu arteritis and rheumatoid arthritis (5,26,27). Serum bilirubin levels were also found to be significantly lower in patient with Crohn’s disease and it was dependent on UDP-glucuronosyl transferase (UGT1A1) allele homozygosity (28). Similarly, in many other AID such as neuromyelitis optica (29) primary biliary cirrhosis (PBC) (30) insulin dependent diabetes mellitus (IDDM) (31), higher bilirubin levels have found to be associated with lesser severity and a favorable prognosis. However, most of these evidences come from retrospective case-control studies, therefore further prospective high-quality cohort studies are needed in order to make full use of the protective characteristics of bilirubin in AID.
Serum bilirubin and cancer
The relationship between serum bilirubin and cancer has been revealed in recent years. Molecular studies on human cancer cells have shown that anticancer effects of bilirubin are due to its ability to drastically increase free radical levels inside the tumor cells, thereby alleviating the oxidative stress. Increased reactive oxygen species damage DNA structure and alters gene expression reducing cell proliferation (32).
In a large prospective study of 68,676 Korean population who were followed for 10 years, serum bilirubin levels consistently showed a protective effect on the risk of development of lung cancer in both never and current smokers. Smokers with bilirubin level 0.2–0.7 mg/dL had 6 times higher risk of development of lung cancer than never-smokers with bilirubin >1.0 mg/dL (33). However, previous studies have demonstrated that smoking is inversely associated with serum bilirubin (34). Wen et al. (35) reported that bilirubin is a risk predictor for increased incidence and mortality of lung cancer in smokers. They found that with every 0.1 mg/dL decrease in bilirubin, incidence and mortality of lung cancer in male smokers increased by 5% and 6%, respectively (P<0.001). Smokers with a history of ≥30 pack years with bilirubin level of <0.75 mg/dL had 31% higher risk of lung cancer when compared to bilirubin level of >1 mg/dL. In a retrospective study on 1,617 patients with curatively resected non-small cell lung cancer, moderately elevated pretreatment bilirubin is associated with improved longer-term survival (36). In a larger cohort study from UK primary care research database (the health improvement network) comprising of 504,206 adults, an inverse association between bilirubin and lung cancer is found. Authors estimated that for every 0.1 mg/dL increase in bilirubin, decrease in incidence rate of lung cancer was 8% (95% CI, 5–11%) in men and 11% (95% CI, 7–14%) in women (37).
In vitro studies have also shown that bilirubin induced apoptosis of colon adenocarcinoma cells by directly dissipating mitochondrial membrane potential and this effect occurs at bilirubin concentration normally present in the intestinal lumen (38). However, clinical and epidemiological studies have shown contradictory results on the effect of bilirubin on colorectal cancer. In a study from NHANES from 1988 to 1994 with 20,216 adult subjects, it was found that each 1 mg/dL increase in bilirubin is associated with decreased prevalence of colon cancer (OR =0.257; 95% CI 0.254–0.260) (39). In a case-control study performed by Jirásková et al., it was showed that patients with sporadic colorectal cancer had lower bilirubin compared to healthy adults and each 0.058 mg/dL (1 µmol/L) decrease in bilirubin is associated with a 7% increase in colorectal cancer risk (P<0.001) (40). In a retrospective case control study, it was found that direct bilirubin level was independently associated with lymph node metastasis in rectal cancer and poor prognosis (41). In a study on NHANES III [1998–1994] data, an inverse correlation between bilirubin levels and history of colorectal cancer is found (39). On the contrary, in another study from NHANES-I [1971–1974], baseline serum total bilirubin concentrations are not associated with the incidence of colorectal cancer (42). The discrepancy in these results could be due to the fasting status of patients, as NHANES-I patients were not asked to fast before the collection of the blood samples as opposed to NHANES III data. In addition, the levels of serum bilirubin have also been used as a biomarker to predict the prognosis in patients with pancreatic cancer (43). In a study of 2,425 newly diagnosed non-metastatic breast cancer in female Caucasians, high bilirubin levels are significantly associated with 5-years over-all survival and nearly 40% reduction in risk of death (HR: 1.42; 95% CI 0.45–0.85) (44). Above studies have shown that bilirubin level could predict prognosis in patients with various cancers but there are no prospective or randomized trials which could conform these results.
Serum bilirubin and T2DM
In recent years, interest has been extended to explore the effect of serum bilirubin on T2DM. Emerging evidence has shown that the serum bilirubin concentrations are related to the development of T2DM and its complications. In a middle aged and elderly Japanese cohort, Deetman et al. (45) found an inverse association between serum bilirubin levels and HbA1C, and prevalence of T2DM. Authors proposed that higher serum concentration of bilirubin suppresses the development of T2DM via its anti-oxidative effects (45). However, Wang et al. performed a cross-sectional analysis in two Chinese cohorts and found that serum bilirubin level does not protect against the development of T1DM and direct bilirubin levels were actually associated with increased risk of T2DM (46).
A negative relationship between serum bilirubin and metabolic syndrome has been found in patients with T2DM (47), and serum bilirubin was found to be associated with glycemic variability in females patients with T2DM (48). In a recent meta-analysis of observational studies on 23,141 subjects and 7,944 patients with diabetic nephropathy, Zhang et al. found that bilirubin in diabetic nephropathy groups is lower than non-diabetic nephropathy group and there is significant negative relationship between bilirubin and the risk of diabetic nephropathy (OR: 0.86; 95% CI 0.82–0.90) (49). Authors proposed that bilirubin could be used as a biomarker of diabetic nephropathy. In another meta-analysis by Hamamoto et al. a negative nonlinear association between bilirubin and the risk of diabetic complications such as diabetic nephropathy, retinopathy and neuropathy is identified (50).
Furthermore, lower serum bilirubin has been reported to be associated with other cardiovascular complications in patients with T2DM, such as autonomic neuropathy, arterial stiffness, peripheral neuropathy, retinopathy and carotid atherosclerosis (51-55). However, data from multiple prospective cohort studies and retrospective case-control studies are conflicting because of the presence of multiple confounders which could affect bilirubin (56).
Serum bilirubin in other human disorders
In addition to the aforementioned diseases, serum bilirubin has also been found to have prognostic value in other diseases. Serum bilirubin has been found to be inversely related to the C-reactive protein in patients with migraine (57), and increased serum bilirubin levels can reduce oxidative stress response in patients with HIV (58). In an interesting study, higher serum bilirubin concentrations were demonstrated to be associated with decreased postoperative liver’s ischemia/reperfusion injury (IRI) in patients with live donor liver transplantation (59). Serum bilirubin has also been proposed to be a useful marker to differentiate cardioembolic stroke from other subtypes of strokes (60). Recently, high serum bilirubin levels were found to be significantly associated with the fatal outcome in patients infected with Ebola virus (61). Serum bilirubin plays a significant role in anti-inflammatory response in patients with psoriasis vulgaris and hypothyroidism disease (62,63). Serum bilirubin is an important biochemical parameter to assess depressive conditions and may improve its complete management (64). However, its protective concentrations may be limited in a certain range.
Conclusions
Bilirubin has an important role in multiple clinical applications and appears to be a promising biological parameter to predict prognosis. It possesses anti-oxidative, anti-inflammatory and immunosuppressive properties (65). In fact, these characteristics have been thought to act as a central link in the pathogenesis of many diseases (3). Hence, we should consider that serum bilirubin is closely related to human health, although its exact mechanism remains largely unknown. Bilirubin is affected by many factors such as smoking, age, gender, fasting status, alcohol use and undiagnosed liver diseases which could be the reason for discrepancies in the results of some of the studies. There is potential heterogeneity due to aforementioned reason in the cut off value of serum bilirubin which could be used in clinical practice. Therefore, there is immense need of larger, prospective and possibly randomized controlled trials to clearly delineate the role of bilirubin in various disease processes.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jlpm.2017.09.08). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tiribelli C, Ostrow JD. The molecular basis of bilirubin encephalopathy and toxicity: report of an EASL Single Topic Conference, Trieste, Italy, 1-2 October, 2004. J Hepatol 2005;43:156-66. [Crossref] [PubMed]
- Kinderlerer AR, Pombo Gregoire I, Hamdulay SS, et al. Heme oxygenase-1 expression enhances vascular endothelial resistance to complement-mediated injury through induction of decay-accelerating factor: a role for increased bilirubin and ferritin. Blood 2009;113:1598-607. [Crossref] [PubMed]
- Peng YF, Wang JL, Pan GG. The correlation of serum bilirubin levels with disease activity in patients with rheumatoid arthritis. Clin Chim Acta 2017;469:187-90. [Crossref] [PubMed]
- Wagner KH, Wallner M, Mölzer C, et al. Looking to the horizon: the role of bilirubin in the development and prevention of age-related chronic diseases. Clin Sci (Lond) 2015;129:1-25. [Crossref] [PubMed]
- Ohnaka K, Kono S, Inoguchi T, et al. Inverse associations of serum bilirubin with high sensitivity C-reactive protein, glycated hemoglobin, and prevalence of type 2 diabetes in middle-aged and elderly Japanese men and women. Diabetes Res Clin Pract 2010;88:103-10. [Crossref] [PubMed]
- Peng YF, Wei YS. Associations between serum bilirubin levels and essential trace elements status in an adult population. Oncotarget 2017; [Epub ahead of print].
- Vítek L. Relationship of bilirubin to diseases caused by increased oxidative stress. Vnitr Lek 2013;59:618-21. [PubMed]
- Schwertner HA, Jackson WG, Tolan G. Association of low serum concentration of bilirubin with increased risk of coronary artery disease. Clin Chem. 1994;40:18-23. [PubMed]
- Breimer LH, Wannamethee G, Ebrahim S, et al. Serum bilirubin and risk of ischemic heart disease in middle-aged British men. Clin Chem 1995;41:1504-8. [PubMed]
- Bulmer AC, Verkade HJ, Wagner KH. Bilirubin and beyond: a review of lipid status in Gilbert's syndrome and its relevance to cardiovascular disease protection. Prog Lipid Res 2013;52:193-205. [Crossref] [PubMed]
- Mahabadi AA, Lehmann N, Möhlenkamp S, et al. Association of bilirubin with coronary artery calcification and cardiovascular events in the general population without known liver disease: the Heinz Nixdorf Recall study. Clin Res Cardiol 2014;103:647-53. [Crossref] [PubMed]
- Kang SJ, Lee C, Kruzliak P. Effects of serum bilirubin on atherosclerotic processes. Ann Med 2014;46:138-47. [Crossref] [PubMed]
- Ko GT, Chan JC, Woo J, et al. Serum bilirubin and cardiovascular risk factors in a Chinese population. J Cardiovasc Risk 1996;3:459-63. [Crossref] [PubMed]
- de Sauvage Nolting PR, Kusters DM, Hutten BA, et al. Serum bilirubin levels in familial hypercholesterolemia: a new risk marker for cardiovascular disease? J Lipid Res 2011;52:1755-9. [Crossref] [PubMed]
- Oda E, Kawai R. A possible cross-sectional association of serum total bilirubin with coronary heart disease and stroke in a Japanese health screening population. Heart Vessels 2012;27:29-36. [Crossref] [PubMed]
- Boon AC, Bulmer AC, Coombes JS, et al. Circulating bilirubin and defense against kidney disease and cardiovascular mortality: mechanisms contributing to protection in clinical investigations. Am J Physiol Renal Physiol 2014;307:F123-36. [Crossref] [PubMed]
- Lin JP, Vitek L, Schwertner HA. Serum bilirubin and genes controlling bilirubin concentrations as biomarkers for cardiovascular disease. Clin Chem 2010;56:1535-43. [Crossref] [PubMed]
- Chang CC, Hsu CY, Huang PH, et al. Association of Serum Bilirubin with SYNTAX Score and Future Cardiovascular Events in Patients Undergoing Coronary Intervention. Acta Cardiol Sin 2016;32:412-9. [PubMed]
- Bakrania B, Du Toit EF, Wagner KH, et al. Pre- or post-ischemic bilirubin ditaurate treatment reduces oxidative tissue damage and improves cardiac function. Int J Cardiol 2016;202:27-33. [Crossref] [PubMed]
- Liu Y, Li P, Lu J, et al. Bilirubin possesses powerful immunomodulatory activity and suppresses experimental autoimmune encephalomyelitis. J Immunol 2008;181:1887-97. [Crossref] [PubMed]
- Fischman D, Valluri A, Gorrepati VS, et al. Bilirubin as a Protective Factor for Rheumatoid Arthritis: An NHANES Study of 2003 - 2006 Data. J Clin Med Res 2010;2:256-60. [PubMed]
- Peng YF, Zhang L, Pan GG, et al. A potential clinical usefulness of measuring serum bilirubin levels in patients with polymyositis. Eur Rev Med Pharmacol Sci 2016;20:631-5. [PubMed]
- Vítek L, Muchová L, Jančová E, et al. Association of systemic lupus erythematosus with low serum bilirubin levels. Scand J Rheumatol 2010;39:480-4. [Crossref] [PubMed]
- Yang Z, Liang Y, Li C, et al. Bilirubin levels in patients with systemic lupus erythematosus: increased or decreased? Rheumatol Int 2012;32:2423-30. [Crossref] [PubMed]
- Peng F, Deng X, Yu Y, et al. Serum bilirubin concentrations and multiple sclerosis. J Clin Neurosci 2011;18:1355-9. [Crossref] [PubMed]
- Yang D, Su Z, Wu S, et al. Low antioxidant status of serum bilirubin, uric acid, albumin and creatinine in patients with myasthenia gravis. Int J Neurosci 2016;126:1120-6. [Crossref] [PubMed]
- Peng YF, Deng YB. Serum Bilirubin Concentrations in Patients With Takayasu Arteritis. Arch Pathol Lab Med 2017;141:846-50. [Crossref] [PubMed]
- Leníček M, Duricová D, Hradsky O, et al. The relationship between serum bilirubin and Crohn's disease. Inflamm Bowel Dis 2014;20:481-7. [Crossref] [PubMed]
- Peng F, Yang Y, Liu J, et al. Low antioxidant status of serum uric acid, bilirubin and albumin in patients with neuromyelitis optica. Eur J Neurol 2012;19:277-83. [Crossref] [PubMed]
- Bonnand AM, Heathcote EJ, Lindor KD, et al. Clinical significance of serum bilirubin levels under ursodeoxycholic acid therapy in patients with primary biliary cirrhosis. Hepatology 1999;29:39-43. [Crossref] [PubMed]
- Nishimura T, Tanaka M, Sekioka R, et al. Serum bilirubin concentration is associated with eGFR and urinary albumin excretion in patients with type 1 diabetes mellitus. J Diabetes Complications 2015;29:1223-7. [Crossref] [PubMed]
- Rao P, Suzuki R, Mizobuchi S, et al. Bilirubin exhibits a novel anti-cancer effect on human adenocarcinoma. Biochem Biophys Res Commun 2006;342:1279-83. [Crossref] [PubMed]
- Lim JE, Kimm H, Jee SH. Combined effects of smoking and bilirubin levels on the risk of lung cancer in Korea: the severance cohort study. PLoS One 2014;9:e103972 [Crossref] [PubMed]
- O'Malley SS, Wu R, Mayne ST, et al. Smoking cessation is followed by increases in serum bilirubin, an endogenous antioxidant associated with lower risk of lung cancer and cardiovascular disease. Nicotine Tob Res 2014;16:1145-9. [Crossref] [PubMed]
- Wen CP, Zhang F, Liang D, et al. The ability of bilirubin in identifying smokers with higher risk of lung cancer: a large cohort study in conjunction with global metabolomic profiling. Clin Cancer Res 2015;21:193-200. [Crossref] [PubMed]
- Li N, Xu M, Cai MY, et al. Elevated serum bilirubin levels are associated with improved survival in patients with curatively resected non-small-cell lung cancer. Cancer Epidemiol 2015;39:763-8. [Crossref] [PubMed]
- Horsfall LJ, Rait G, Walters K, et al. Serum bilirubin and risk of respiratory disease and death. JAMA 2011;305:691-7. [Crossref] [PubMed]
- Keshavan P, Schwemberger SJ, Smith DL, et al. Unconjugated bilirubin induces apoptosis in colon cancer cells by triggering mitochondrial depolarization. Int J Cancer 2004;112:433-45. [Crossref] [PubMed]
- Zucker SD, Horn PS, Sherman KE. Serum bilirubin levels in the U.S. population: gender effect and inverse correlation with colorectal cancer. Hepatology 2004;40:827-35. [Crossref] [PubMed]
- Jirásková A, Novotný J, Novotný L, et al. Association of serum bilirubin and promoter variations in HMOX1 and UGT1A1 genes with sporadic colorectal cancer. Int J Cancer 2012;131:1549-55. [Crossref] [PubMed]
- Gao C, Fang L, Li JT, et al. Significance and prognostic value of increased serum direct bilirubin level for lymph node metastasis in Chinese rectal cancer patients. World J Gastroenterol 2016;22:2576-84. [Crossref] [PubMed]
- Ioannou GN, Liou IW, Weiss NS. Serum bilirubin and colorectal cancer risk: a population-based cohort study. Aliment Pharmacol Ther 2006;23:1637-42. [Crossref] [PubMed]
- Haas M, Heinemann V, Kullmann F, et al. Prognostic value of CA 19-9, CEA, CRP, LDH and bilirubin levels in locally advanced and metastatic pancreatic cancer: results from a multicenter, pooled analysis of patients receiving palliative chemotherapy. J Cancer Res Clin Oncol 2013;139:681-9. [Crossref] [PubMed]
- Liu X, Meng QH, Ye Y, et al. Prognostic significance of pretreatment serum levels of albumin, LDH and total bilirubin in patients with non-metastatic breast cancer. Carcinogenesis 2015;36:243-8. [Crossref] [PubMed]
- Deetman PE, Kwakernaak AJ, Bakker SJ, et al. Low-normal free thyroxine confers decreased serum bilirubin in type 2 diabetes mellitus. Thyroid 2013;23:1367-73. [Crossref] [PubMed]
- Wang J, Li Y, Han X, et al. Serum bilirubin levels and risk of type 2 diabetes: results from two independent cohorts in middle-aged and elderly Chinese. Sci Rep 2017;7:41338. [Crossref] [PubMed]
- Nano J, Muka T, Cepeda M, et al. Association of circulating total bilirubin with the metabolic syndrome and type 2 diabetes: A systematic review and meta-analysis of observational evidence. Diabetes Metab 2016;42:389-97. [Crossref] [PubMed]
- Kim LK, Roh E, Kim MJ, et al. Serum bilirubin levels are positively associated with glycemic variability in women with type 2 diabetes. J Diabetes Investig 2016;7:874-80. [Crossref] [PubMed]
- Zhang D, Zhu B, Zhang W, et al. Total bilirubin level may be a biomarker of nephropathy in type 2 diabetes mellitus: A meta-analysis of observational studies based on MOOSE compliant. Medicine (Baltimore) 2017;96:e5765 [Crossref] [PubMed]
- Hamamoto S, Kaneto H, Kamei S, et al. Low bilirubin levels are an independent risk factor for diabetic retinopathy and nephropathy in Japanese patients with type 2 diabetes. Diabetes Metab 2015;41:429-31. [Crossref] [PubMed]
- Chung JO, Cho DH, Chung DJ, et al. Physiological serum bilirubin concentrations are inversely associated with the prevalence of cardiovascular autonomic neuropathy in patients with Type 2 diabetes. Diabet Med 2014;31:185-91. [Crossref] [PubMed]
- Kim ES, Mo EY, Moon SD, et al. Inverse association between serum bilirubin levels and arterial stiffness in Korean women with type 2 diabetes. PLoS One 2014;9:e109251 [Crossref] [PubMed]
- Kim ES, Lee SW, Mo EY, et al. Inverse association between serum total bilirubin levels and diabetic peripheral neuropathy in patients with type 2 diabetes. Endocrine 2015;50:405-12. [Crossref] [PubMed]
- Dave A, Kalra P, Gowda BH, et al. Association of bilirubin and malondialdehyde levels with retinopathy in type 2 diabetes mellitus. Indian J Endocrinol Metab 2015;19:373-7. [Crossref] [PubMed]
- Kawamoto R, Ninomiya D, Hasegawa Y, et al. Mildly elevated serum total bilirubin levels are negatively associated with carotid atherosclerosis among elderly persons with type 2 diabetes. Clin Exp Hypertens 2016;38:107-12. [Crossref] [PubMed]
- Breimer LH, Mikhailidis DP. Does bilirubin protect against developing diabetes mellitus? J Diabetes Complications 2016;30:728-37. [Crossref] [PubMed]
- Peng YF, Xie LQ, Xiang Y, et al. Serum Bilirubin and Their Association With C-Reactive Protein in Patients With Migraine. J Clin Lab Anal 2016;30:982-5. [Crossref] [PubMed]
- Estrada V, Monge S, Gómez-Garre MD, et al. Relationship between plasma bilirubin level and oxidative stress markers in HIV-infected patients on atazanavir- vs. efavirenz-based antiretroviral therapy. HIV Med 2016;17:653-61. [Crossref] [PubMed]
- Spetzler VN, Goldaracena N, Kaths JM, et al. High preoperative bilirubin values protect against reperfusion injury after live donor liver transplantation. Transpl Int 2015;28:1317-25. [Crossref] [PubMed]
- Lin SP, Lin PY, Jiang HL, et al. Is serum total bilirubin useful to differentiate cardioembolic stroke from other stroke subtypes? Neurol Res 2015;37:727-31. [Crossref] [PubMed]
- Cournac JM, Karkowski L, Bordes J, et al. Rhabdomyolysis in Ebola Virus Disease. Results of an Observational Study in a Treatment Center in Guinea. Clin Infect Dis 2016;62:19-23. [Crossref] [PubMed]
- Zhou ZX, Chen JK, Hong YY, et al. Relationship Between the Serum Total Bilirubin and Inflammation in Patients With Psoriasis Vulgaris. J Clin Lab Anal 2016;30:768-75. [Crossref] [PubMed]
- Roy S, Banerjee U, Dasgupta A. Protective Role of Bilirubin Against Increase in hsCRP in Different Stages of Hypothyroidism. Indian J Clin Biochem 2016;31:43-9. [Crossref] [PubMed]
- Peng YF, Xiang Y, Wei YS. The significance of routine biochemical markers in patients with major depressive disorder. Sci Rep 2016;6:34402. [Crossref] [PubMed]
- Gazzin S, Vitek L, Watchko J, et al. A Novel Perspective on the Biology of Bilirubin in Health and Disease. Trends Mol Med 2016;22:758-68. [Crossref] [PubMed]
Cite this article as: Peng YF, Goyal H, Xu GD. Serum bilirubin has an important role in multiple clinical applications. J Lab Precis Med 2017;2:82.