
Get FIT for the new year: a review of the role of faecal immunochemical test for haemoglobin in patients with symptoms of colorectal disease
Introduction
In 2012, there were 1,361,000 colorectal cancer (CRC) cases registered worldwide (1). CRC is the third most common cancer in men (746,000 cases) and the second in women (614,000 cases) worldwide. Despite the rising number of newly diagnosed cases of CRC, mortality has generally decreased over the past 40 years (1). Colonoscopy as a gold standard is undisputed in the diagnosis of CRC in both symptomatic and asymptomatic individuals. However, colonoscopy, being an invasive procedure, is not without risk, albeit that serious complications such as bleeding [2.6/1,000 procedures, 95% confidence interval (CI): 1.7–3.7] and perforation (0.5/1,000 procedures, 95% CI: 0.4–0.7) are low (2). In addition, the procedure is time-consuming and involves a significant input from heath care professionals. Whilst screening has impacted positively on the health of asymptomatic participants, there is still a large number of cases of CRC that present with symptoms, mainly in primary care but also in secondary care (3). Differentiating the patients with serious pathology [CRC + higher-risk (advanced) adenoma (HRA) + inflammatory bowel disease (IBD)] from those with benign or functional colorectal disease can be a challenge due to the major overlap of symptoms.
The need for reliable rule-out criteria
The early diagnosis of CRC in patients presenting with symptoms of colorectal disease may improve prognosis (4). Several risk classification scores based on symptoms have been developed to address this. National Institute for Health and Care Excellence (NICE) (4) and Scottish Intercollegiate Guidelines Network (SIGN) (5) recommendations are only two examples of such guidelines. These classification criteria are intended to assess which patients are most at risk of having CRC, and thus prioritise these patients for colonoscopy—shorten this sentence. There is, however, the need for a simple, inexpensive rule-out tool to help alleviate the resulting burden on endoscopic services and prioritise these patients (6).
The 2-week wait referral guideline was introduced by the National Health Service in England (NHSE) and has been implemented in most centres; however, compliance with this guideline has not been good (7). Additionally, this system has had an adverse impact on the waiting times for routine referrals for investigation of the colorectum (7). In fact, only 24% of incident CRC cases were diagnosed through the 2-week wait strategy and no evidence was found that these CRC cases were diagnosed at an earlier stage (8). Jellema et al. (9) evaluated the diagnostic accuracy of the 2-week wait criteria, and found that the sensitivity and specificity for CRC detection are 92% and 42%, respectively. In this study, the available evidence on diagnostic tests accessible in primary care to identify which patients with symptoms had an increased probability of having CRC was evaluated. Patient age, being on the referral arm of a clinical guideline, and a positive faecal immunochemical test for haemoglobin (FIT) result are identified as highly sensitive factors. FIT also has good specificity, as does a positive family history, unexplained weight loss and iron deficiency anaemia (Table 1).
Table 1
| Index investigation | Sensitivity (%) | Specificity (%) | PPV (%) |
|---|---|---|---|
| gFOBT | 75 | 86 | 28 |
| FIT | 95 | 84 | 21 |
| Family history | 16 | 91 | 6 |
| Weight loss | 20 | 89 | 9 |
| Iron deficiency anaemia | 13 | 92 | 13 |
Adapted from Jellema et al. (9). gFOBT, guaiac-based faecal occult blood test; FIT, biochemistry and terminology; CRC, colorectal cancer; PPV, positive predictive value.
Only a small proportion of the haem moiety of haemoglobin that finds its way into the upper gastro-intestinal tract lumen undergoes degradation; the major portion enters the colon intact. In the lower gastro-intestinal tract, intact haem, together with any haem of haemoproteins shed directly into the colonic lumen as haemoglobin or other haemoproteins, is converted by bacteria to a range of haem-derived porphyrins lacking iron (10). This conversion is a slow and incomplete process and the amount converted in this way depends on colonic transit rate, site of bleeding and amount of luminal haem (10). Following this process, faeces will contain a heterogeneous mixture of intact haemoglobin, intact haem, as well as globin and haem derived porphyrins - the stage of degradation depending on the location of bleeding in the gut (10). In the presence of CRC, this mixture will contain higher concentrations of all the products (10). Fraser et al. (11) analysed the faecal haemoglobin concentration [f-Hb; measured in µg Hb/g—the standard unit of measurement proposed (12)] in a number of colonoscopy groups, subdividing the subjects by the pathology found at colonoscopy. They clearly demonstrated a difference in f-Hb between cancer and other colonic pathologies (Figure 1).

The traditional guaiac-based faecal occult blood test (gFOBT) is based on the peroxidase activity of the haem moiety of haemoglobin. In our opinion, this technique has inherent disadvantages such as issues with sample transfer onto the specimen collection cards, interference of dietary constituents and non-specificity for gastro-intestinal origin of bleeding. gFOBT is therefore not suitable for symptomatic patients. The Expert Working Group of the CRC Screening Committee, World Endoscopy Organization, “FIT for Screening” advocate the use of the terminology FIT to distinguish this from other methods for detection of the presence of blood in faeces (12). In contrast to gFOBT, FIT is more compliant-friendly—since only one sample is required—sampling of faeces is done using user-friendly specimen collection devices and the results are not affected by constituents of consumed food. Moreover, globin in haemoglobin is digested by proteolytic enzymes in the gut, hence upper gastro-intestinal bleeding is not detected, making FIT more specific to the colorectum (10). Therefore, FIT is selective for colorectal bleeding since globin from the upper gastro-intestinal tract is not present in significant amount in faeces (10). A study by Young et al. showed that ingested blood of up to 100 mL was not detected by some immunochemical methods but was by gFOBT (13). FIT is not clinically specific, however, because non-neoplastic and benign pathologies may also bleed and certainly the dogma is that there is a small concentration of haemoglobin in faeces that reflects usual physiological blood loss (14).
The immunoassay methods differ between qualitative and quantitative FIT (12). FIT assays can be carried out in a number of techniques: qualitative FIT generally use lateral flow immunochromatographic analysis [as used in many point-of-care (POC) devices] and quantitative FIT generally use laboratory-based immunoturbidimetry on small closed bench top analysers.
Qualitative FIT
Qualitative FIT use test cassettes or strips, in which separation of haemoglobin occurs using lateral flow and is captured by antibodies to the globin component. Qualitative FIT devices can be used as POC tests as well as in opportunistic clinical settings. The f-Hb concentration that is used as the cut-off between negative and positive in such tests is set by the manufacturer and these cut-offs differ considerably giving lack of consistency of clinical outcomes (15,16). Steele et al. (17) state that they are not easy tests to use in the ambulatory setting, because, amongst other difficulties, they require skill and practice to obtain consistency in sample application and visual interpretation
Kok et al. (18) assessed the ability of faecal biomarkers [faecal calprotectin (f-C) and qualitative FIT] to differentiate between organic bowel disease—which included IBD, CRC and all adenomas—and non-organic bowel disease in symptomatic patients in primary care. They found an NPV of 81% for f-C and 84% for FIT in their cohort of 386 patients, thereby proving that both biomarkers are useful for ruling out CRC. Elias et al. (19). reported that when f-C and FIT were incorporated into a diagnostic model which also factored in patient clinical data, an NPV for significant colorectal disease of 96.4% is achieved.
Szilagyi et al. (20) assessed qualitative FIT performance against colonoscopy results in a cohort of 144 patients. Five advanced adenomas [without high-grade dysplasia (HDG) or adenocarcinoma] and several cases of multiple adenomas were missed in the group with FIT negative test results. Sensitivity, specificity and NPV for advanced polyps are 63.6%, 82.7% and 96.5%, respectively.
In a study by Digby et al. (21), f-Hb concentration is correlated with stage of CRC and adenoma. Polyp cancers have lower concentrations than more advanced stage cancers (P<0.04), with HRA having significantly higher f-Hb concentrations than low risk adenomas (LRA): f-Hb, therefore, is related to severity of colorectal neoplasia.
A CRC which bleeds intermittently might be one of the reasons for a false negative FIT result. In a recent publication, the effectiveness of different numbers of samples for a POC FIT in symptomatic patients with CRC or adenomas with HDG in the primary care setting was assessed (22). In this study, three FITs (with at least one positive FIT result) detected 13 more cases than a single FIT in a cohort of 139 cases with CRC or adenomas with HGD. This means that a single negative qualitative FIT may not be adequately reassuring.
Quantitative FIT
Quantitative FITs generally use immunoturbidimetric methods, providing a measure of haemoglobin in faeces captured in a buffer solution within the specimen collection device. The amount of faeces sampled will therefore affect the measured concentration. However, studies have shown that the f-Hb concentration is also—and more greatly so—related to the severity of the neoplastic pathology present (11,14,23,24). Therefore, when neoplasia is present, there will be more bleeding, and this will be reflected in the found f-Hb. Subsequently, it is also important to determine at what point—or, more accurately, cut-off—FIT is to be considered positive. Data on assessment of symptomatic patients using different f-Hb cut-offs are available in the literature (25,26). Whilst the cut-off is important, it should probably be set dependent on the population to be assessed and the prevalence of CRC. For the population in England, NICE recommend a f-Hb cut-off of 10 µg Hb/g faeces in the recent DG30 diagnostic guidance (27).
Quantitative FITs have major advantages over qualitative FIT and gFOBT. The end point is an objective result, which can be more easily compared and stratified and is more amenable to quality assurance procedures. There are a number of commercially available FIT analytical systems. NICE (27) currently recommends the use of OC-sensor, HM-JACKarc or FOB Gold quantitative procedures: “for suspected CRC in people without rectal bleeding who have unexplained symptoms but do not meet the criteria for a suspected cancer pathway referral outlined in NICE’s NG12 guideline.”
The various FIT collection devices and analytical systems have been compared in a recent review (28) and a number of points have been highlighted: FIT manufacturers continually evolve their products; hence outcomes might not be comparable over time. There is, however, a push for standardisation of reporting of the results obtained with FIT (29,30).
There is an age and sex difference in f-Hb, with that in males and the elderly being higher than that in females and the younger subjects (31). This could potentially lead to the need for different f-Hb cut-offs based on sex and age. A prospective cohort study showed that a cut-off of 10 µg Hb/g faeces gives similar results in both sexes, at least in terms of positive predictive value (PPV) (32).
FIT and other biomarkers
There are a number of biomarkers that have been suggested as being useful in the evaluation of symptomatic patients. These include blood haemoglobin [iron deficiency anaemia—92% specific for CRC, albeit poorly sensitive (10,33)], f-Hb concentration, serum carcinoembryonic antigen (CEA) but with poor sensitivity and specificity for diagnosis (34) and f-C (35).
f-C has been shown to be a good marker in colorectal pathologies of an inflammatory nature (36,37) and concentrations have been found to be significantly elevated also in neoplastic conditions. In a recent study, Turvill et al. (35), investigated the role of f-C as a primary care assessment for CRC in patients with lower gastro-intestinal symptoms. In their diagnostic accuracy study, f-C had a high NPV for CRC in patients with suspected CRC: 27.8% of patients referred for colonoscopy via the 2-week wait criteria had a negative f-C result and a negative colonoscopy.
CRC asymptomatic population screening with gFOBT in average-risk populations significantly reduces CRC mortality (38). However, several studies comparing gFOBT and FIT for the detection of CRC and advanced adenomas have shown FIT to be more sensitive and specific for their detection (13,23,39). In contrast, there is little literature on the role of these biomarkers in assessment of symptomatic patients. Going back to the meta-analysis published by Jellema et al. (9), FIT had high sensitivity and specificity for CRC detection and NPV of 100%. Unfortunately, however, this meta-analysis included studies with both asymptomatic and symptomatic cohorts. Mowat et al. (40) investigated FIT and f-C in a cohort of 1,043 symptomatic patients, in the primary care setting. The diagnostic accuracies of f-Hb and f-C for identification of significant colorectal disease were assessed by comparing these to the colonoscopy result. The negative predictive values of FIT for CRC and HRA were 100% and 97.8%, respectively. Undetectable f-Hb measured in samples collected in primary care proved a good “rule-out test” for significant colorectal disease: CRC was excluded, and HRAs were rare: interestingly, f-C less than 50 µg/g missed five CRC and 17 high-risk adenoma cases. Widlak et al. (41) recently assessed the use of FIT or f-C to detect CRC and adenoma in symptomatic patients who had fulfilled the NHSE 2-week wait referral criteria. In their study, undetectable f-Hb had an NPV of 100% for exclusion of CRC, with higher f-Hb concentrations in left-sided lesions. Performing f-C in addition did not confer any benefits.
Of the biomarkers mentioned above, therefore, FIT appears to be the most promising tool for the prioritisation of further investigation for CRC in symptomatic patients.
Where does FIT fit in clinical practice?
With the value of FIT in CRC screening already well established, a number of studies set out to address the topic of the role of FIT in assessing symptomatic patients for the risk of CRC and other serious colorectal disease (HRA + IBD) and the following review of the available literature highlights important points in this regard.
McDonald et al. (42) assessed the NPV of FIT in 280 patients with lower abdominal symptoms—100% for cancer and 94.4% for HRA—concluding that the use of f-Hb measurements can contribute to reducing unnecessary endoscopy for symptomatic patients. Therefore, FIT was a useful rule-out test in this cohort of patients. Godber et al. (43) investigated 909 patients referred from primary care for colonoscopy: 484 patients submitted a sample for f-Hb and underwent a colonoscopy. Using a cut-off of 10 µg Hb/g faeces, NPV was 96.2% for significant colorectal disease. All patients with CRC (n=11, 2.2%), had a high f-Hb concentration, with the resultant clinical sensitivity being 100%. A cut-off of f-Hb of less than 10 µg Hb/g faeces measured in samples collected in primary care proved a good “rule-out test” for significant colorectal disease in the aforementioned Mowat et al. study (40), with an NPV of 99.5% for CRC and of 96.5% for HRA. Kaul et al. (44) demonstrated a use for qualitative FIT set at a cut-off of 10 µg Hb/g faeces. In this study, they scrutinised all 2-week wait referrals, to ensure that they all accurately reflected the correct referral criteria. No cancers were missed (NPV 100%) (Table 2). However, if patients met clinical referral criteria and were FIT positive, there was a 60% (n=18/30) chance of having a cancer.
Table 2
| Colonic pathology | FIT positive | FIT negative |
|---|---|---|
| Adenocarcinoma | 17 | 0 |
| Squamous cell carcinoma | 1 | 0 |
| Adenomatous polyp | 1 | 4 |
| Diverticulosis | 6 | 45 |
| Crohn’s disease | 0 | 1 |
| Solitary rectal ulcer | 0 | 1 |
| No pathology | 5 | 31 |
| Total | 30 | 82 |
Adapted from Kaul et al. (44).
Cubiella et al. (45) compared the sensitivity and specificity of FIT in detection of CRC with the then existing NICE (CG27) and SIGN 126 guidelines. FIT at a f-Hb concentration cut-off of 20 µg Hb/g faeces is more accurate for detection of CRC in symptomatic patients, with a sensitivity of 87.6% (NICE: 61.9%; SIGN: 77.4%) and a specificity of 77.4% (NICE: 65%, SIGN: 42%). Auge et al. (25) demonstrated the gender difference in sensitivity and PPV of FIT in symptomatic patients with CRC and advanced adenomas. In their study, utilising two samples collected for FIT per patient, they found that PPV is higher and NPV is lower in males, highlighting the possible need for sex-based cut-offs. Rodríguez-Alonso et al. (46) compared quantitative FIT with NICE CG27 and SIGN 126 guidelines for referral. A cohort of 1,054 symptomatic patients referred for colonoscopy was investigated prospectively. NICE and SIGN guidelines detect 46.7% and 43.3% of cases of CRC whilst FIT detected 96.7% of cases at a cut-off of 15 µg Hb/g faeces. Male sex, age and f-Hb are independent predictive factors of advanced neoplasia and the authors concluded that a score that combines sex, age and f-Hb could accurately estimate the risk of advanced neoplasia. Widlak et al. (41) investigated f-Hb and f-C as biomarkers to identify high-risk patients who were referred via the NHSE 2-week wait criteria: therefore, this study was done in the secondary care setting. A total of 430 patients were assessed, with 24 patients having CRC. FIT sensitivity and specificity for CRC detection are 84% and 93% respectively, at a f-Hb cut-off of 7 µg Hb/g faeces. NPV is 99% for CRC.
FIT in multivariate scoring systems
FIT should not be used in isolation, but should form part of the multi-factorial assessment of the symptomatic patient. Risk-prediction models for CRC risk aim to identify those patients who need further investigation. Cubiella et al. (47) developed, and externally validated, a prediction model in symptomatic patients including f-Hb. This prediction model was shown to have high diagnostic accuracy (Figures 2,3); however, it is a complex model that includes eleven variables.
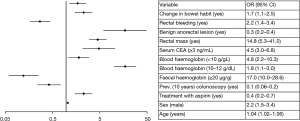
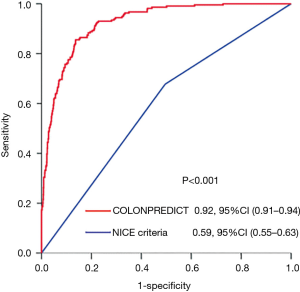
In a more recent effort, these investigators and others from Spain and Scotland simplified this model and suggest that the multivariate FAST Score is an easy to calculate prediction tool (48)—based on f-Hb concentration, sex and age—for detection of CRC in symptomatic patients. They externally validated this score, using data from a study in Spain [Rodríguez-Alonso et al. (46)] and three studies in Scotland [McDonald et al. (42), Godber et al. (43) and Mowat et al. (40)]. Interestingly, the characteristics of the FAST Score were independent of country and FIT analytical system used.
Safety-netting
A f-Hb concentration above the analytical limit of detection is a good rule-out test for significant colorectal disease (42). A positive qualitative FIT result or a quantitative FIT result above the analytical limit of quantitation are unequivocal results and should prompt further investigation. However, the question arises: what about symptomatic patients with negative FIT results: should these be denied further investigation?
The high NPV of FIT for CRC and other significant colorectal disease in symptomatic patients when using a cut-off of 10 µg Hb/g faeces, demonstrating that the likelihood of symptoms originating from the colon in subjects with f-Hb lower than the cut-off applied is low. In this scenario, it is likely that extra-colonic pathology might be the cause for persisting symptoms and that there is no significant luminal disease. Therefore, cross-sectional imaging will give a greater diagnostic yield. There are no studies looking into this yet, and it would be worthwhile assessing what the outcomes of such a patient cohort are in future work.
It is inevitable that—even at a cut-off of 10 µg Hb/g faeces—a minority of CRC and some HRA and IBD will be missed. There should, therefore, be robust application of safety-netting, whereby patients with persisting symptoms should not be dismissed from primary care. Such exceptions should either be re-assessed—with or without a repeat FIT—or be referred to secondary care for further assessment and/or cross-sectional imaging.
Conclusions
FIT is a useful rule-out test for significant colorectal disease, the use of which should perhaps not be in isolation, but with clinical judgement and the results of other examinations such as abdominal and rectal examination and full blood count. There is a definite role for FIT in both the primary and the secondary care setting, but there is a need for guidance on FIT result interpretation and safety-netting should be mandatory. Further studies are required to assess the use of qualitative FIT in primary and secondary care and risk-scoring models incorporating f-Hb should be evaluated and further developed.
Acknowledgments
Prof. CG Fraser is gratefully acknowledged for manuscript revision.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Laboratory and Precision Medicine for the series “Faecal Testing”. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jlpm.2018.05.05). The series “Faecal Testing” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- GLOBOCAN 2012. Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Available online: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx
- Vermeer NC, Snijders HS, Holman FA, et al. Colorectal cancer screening: systematic review of screen-related morbidity and mortality. Cancer Treat Rev 2017;54:87-98. [Crossref] [PubMed]
- Mansouri D, McMillan DC, Crearie C, et al. Temporal Trends in Mode, Site and Stage of Presentation with the Introduction of Colorectal Cancer Screening: A Decade of Experience from the West of Scotland. Br J Cancer 2015;113:556-61. [Crossref] [PubMed]
- National Institute for Health and Care Excellence. NICE Guideline NG12. Available online: https://www.nice.org.uk/guidance/ng12/chapter/1-Recommendations-organised-by-site-of-cancer#lower-gastrointestinal-tract-cancers
- Scottish Intercollegiate Guidelines Network. October 2015. SIGN 126 Diagnosis and Management of Colorectal Cancer. Available online: http://www.sign.ac.uk/sign-126-diagnosis-and-management-of-colorectal-cancer.html
- Vega P, Valentín F, Cubiella J. Colorectal Cancer Diagnosis: Pitfalls and Opportunities. World J Gastrointest Oncol 2015;7:422-33. [Crossref] [PubMed]
- Rai S, Kelly MJ. Prioritization of Colorectal Referrals: A Review of the 2-Week Wait Referral System. Colorectal Dis 2007;9:195-202. [Crossref] [PubMed]
- Thorne K, Hutchings HA, Elwyn G. The effects of the Two-Week Rule on NHS colorectal cancer diagnostic services: a systematic literature review. BMC Health Serv Res 2006;6:43. [Crossref] [PubMed]
- Jellema P, van der Windt DA, Bruinvels DJ, et al. Value of Symptoms and Additional Diagnostic Tests for Colorectal Cancer in Primary Care: Systematic Review and Meta-Analysis. BMJ 2010;340:c1269. [Crossref] [PubMed]
- Young GP, St John DJ, Rose IS, et al. Haem in the Gut. Part II. Faecal Excretion of Haem and Haem-Derived Porphyrins and Their Detection. J Gastroenterol Hepatol 1990;5:194-203. [Crossref] [PubMed]
- Fraser CG, Mathew CM, McKay K, et al. Automated immunochemical quantitation of haemoglobin in faeces collected on cards for screening for colorectal cancer. Gut 2008;57:1256-60. [Crossref] [PubMed]
- Allison JE, Fraser CG, Halloran SP, et al. Comparing Faecal Immunochemical Tests: Improved Standardization Is Needed. Gastroenterology 2012;142:422-4. [Crossref] [PubMed]
- Young GP, Symonds EL, Allison JE, et al. Advances in Faecal Occult Blood Tests: The FIT Revolution. Dig Dis Sci 2015;60:609-22. [Crossref] [PubMed]
- Levi Z, Hazazi R, Rozen P, et al. A quantitative immunochemical faecal occult blood test is more efficient for detecting significant colorectal neoplasia than a sensitive guaiac test. Aliment Pharmacol Ther 2006;23:1359-64. [Crossref] [PubMed]
- Fraser CG. Interpretation of faecal haemoglobin concentration data in colorectal cancer screening and in assessment of symptomatic patients. J Lab Precis Med 2017;2:96. [Crossref]
- Tao S, Seiler CM, Ronellenfitsch U, et al. Comparative Evaluation of Nine Faecal Immunochemical Tests for the Detection of Colorectal Cancer. Acta Oncol 2013;52:1667-75. [Crossref] [PubMed]
- Steele RJ, Fraser CG. Faecal Immunochemical Tests (FIT) for Haemoglobin for Timely Assessment of Patients with Symptoms of Colorectal Disease in Timely Diagnosis of Colorectal Cancer. Cham: Springer International Publishing, 2018:39-66.
- Kok L, Elias SG, Witteman BJ, et al. Diagnostic accuracy of point-of-care fecal calprotectin and immunochemical occult blood tests for diagnosis of organic bowel disease in primary care: the Cost-Effectiveness of a Decision Rule for Abdominal Complaints in Primary Care (CEDAR) study. Clin Chem 2012;58:989-98. [Crossref] [PubMed]
- Elias SG, Kok L, de Wit NJ, et al. Is There an Added Value of Faecal Calprotectin and Haemoglobin in the Diagnostic Work-up for Primary Care Patients Suspected of Significant Colorectal Disease? A Cross-Sectional Diagnostic Study. BMC Med 2016;14:141. [Crossref] [PubMed]
- Szilagyi A, Xue X. Evaluation of a Faecal Immunochemistry Test Prior to Colonoscopy for Outpatients with Various Indications. Clin Exp Gastroenterol 2017;10:285-92. [Crossref] [PubMed]
- Digby J, Fraser CG, Carey FA, et al. Faecal Haemoglobin Concentration Is Related to Severity of Colorectal Neoplasia. J Clin Pathol 2013;66:415-9. [Crossref] [PubMed]
- Högberg C, Söderström L, Lilja M. Faecal Immunochemical Tests for the Diagnosis of Symptomatic Colorectal Cancer in Primary Care: The Benefit of More than One Sample. Scand J Prim Health Care 2017;35:369-72. [Crossref] [PubMed]
- Hol L, Wilschut JA, van Ballegooijen M, et al. Screening for Colorectal Cancer: Random Comparison of Guaiac and Immunochemical Faecal Occult Blood Testing at Different Cut-off Levels. Br J Cancer 2009;100:1103-10. [Crossref] [PubMed]
- de Wijkerslooth TR, Stoop EM, Bossuyt PM, et al. Immunochemical Fecal Occult Blood Testing Is Equally Sensitive for Proximal and Distal Advanced Neoplasia. Am J Gastroenterol 2012;107:1570-8. [Crossref] [PubMed]
- Auge JM, Fraser CG, Rodriguez C, et al. Clinical Utility of One versus Two Faecal Immunochemical Test Samples in the Detection of Advanced Colorectal Neoplasia in Symptomatic Patients. Clin Chem Lab Med 2016;54:125-32. [Crossref] [PubMed]
- Brenner H, Werner S. Selecting a Cut-off for Colorectal Cancer Screening With a Fecal Immunochemical Test. Clin Transl Gastroenterol 2017;8:e111 [Crossref] [PubMed]
- National Institute for Health and Care Excellence. Quantitative Faecal Immunochemical Tests to Guide Referral for Colorectal Cancer in Primary Care. Available online: https://www.nice.org.uk/guidance/dg30
- Fraser CG. Comparison of Quantitative Faecal Immunochemical Tests for Haemoglobin (FIT) for Asymptomatic Population Screening. Transl Cancer Res 2016;5:S916-9. [Crossref]
- Fraser CG, Halloran SP, Allison JE, et al. Making Colorectal Cancer Screening FITTER for Purpose with Quantitative Faecal Immunochemical Tests for Haemoglobin (FIT). Clin Chem Lab Med 2013;51:2065-7. [Crossref] [PubMed]
- Fraser CG, Allison JE, Young GP, et al. Improving the Reporting of Evaluations of Faecal Immunochemical Tests for Haemoglobin: The FITTER Standard and Checklist. Eur J Cancer Prev 2015;24:24-6. [Crossref] [PubMed]
- Fraser CG, Rubeca T, Rapi S, et al. Faecal Haemoglobin Concentrations Vary with Sex and Age, but Data Are Not Transferable across Geography for Colorectal Cancer Screening. Clin Chem Lab Med 2014;52:1211-6. [Crossref] [PubMed]
- Kapidzic A, van der Meulen MP, Hol L, et al. Gender Differences in Fecal Immunochemical Test Performance for Early Detection of Colorectal Neoplasia. Clin Gastroenterol Hepatol 2015;13:1464-71.e4. [Crossref] [PubMed]
- Ford AC, Veldhuyzen van Zanten SJ, Rodgers CC, et al. Diagnostic Utility of Alarm Features for Colorectal Cancer: Systematic Review and Meta-Analysis. Gut 2008;57:1545-53. [Crossref] [PubMed]
- Labianca R, Nordlinger B, Beretta GD, et al. Early colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2013;24:vi64-72. [Crossref] [PubMed]
- Turvill J, Aghahoseini A, Sivarajasingham N, et al. Faecal Calprotectin in Patients with Suspected Colorectal Cancer: A Diagnostic Accuracy Study. Br J Gen Pract 2016;66:e499-506. [Crossref] [PubMed]
- Jellema P, van Tulder MW, van der Horst HE, et al. Inflammatory Bowel Disease: A Systematic Review on the Value of Diagnostic Testing in Primary Care. Colorectal Dis 2011;13:239-54. [Crossref] [PubMed]
- Waugh N, Cummins E, Royle P, et al. Faecal Calprotectin Testing for Differentiating amongst Inflammatory and Non-Inflammatory Bowel Diseases: Systematic Review and Economic Evaluation. Health Technol Assess 2013;17:xv-xix, 1-211. [Crossref] [PubMed]
- Hewitson P, Glasziou P, Watson E, et al. Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (hemoccult): an update. Am J Gastroenterol 2008;103:1541-9. [Crossref] [PubMed]
- Guittet L, Bouvier V, Mariotte N, et al. Comparison of a Guaiac Based and an Immunochemical Faecal Occult Blood Test in Screening for Colorectal Cancer in a General Average Risk Population. Gut 2007;56:210-4. [Crossref] [PubMed]
- Mowat C, Digby J, Strachan JA, et al. Faecal Haemoglobin and Faecal Calprotectin as Indicators of Bowel Disease in Patients Presenting to Primary Care with Bowel Symptoms. Gut 2016;65:1463-9. [Crossref] [PubMed]
- Widlak MM, Thomas CL, Thomas MG, et al. Diagnostic accuracy of faecal biomarkers in detecting colorectal cancer and adenoma in symptomatic patients. Aliment Pharmacol Ther 2017;45:354-63. [Crossref] [PubMed]
- McDonald PJ, Digby J, Innes C, et al. Low Faecal Haemoglobin Concentration Potentially Rules out Significant Colorectal Disease. Colorectal Dis 2013;15:e151-9. [Crossref] [PubMed]
- Godber IM, Todd LM, Fraser CG, et al. Use of a Faecal Immunochemical Test for Haemoglobin Can Aid in the Investigation of Patients with Lower Abdominal Symptoms. Clin Chem Lab Med 2016;54:595-602. [Crossref] [PubMed]
- Kaul A, Shah A, Magill FH, et al. Immunological faecal occult blood testing: A discriminatory test to identify colorectal cancer in symptomatic patients. Int J Surg 2013;11:329-31. [Crossref] [PubMed]
- Cubiella J, Salve M, Díaz-Ondina M, et al. Diagnostic Accuracy of the Faecal Immunochemical Test for Colorectal Cancer in Symptomatic Patients: Comparison with NICE and SIGN Referral Criteria. Colorectal Dis 2014;16:O273-82. [Crossref] [PubMed]
- Rodríguez-Alonso L, Rodríguez-Moranta F, Ruiz-Cerulla A, et al. An Urgent Referral Strategy for Symptomatic Patients with Suspected Colorectal Cancer Based on a Quantitative Immunochemical Faecal Occult Blood Test. Dig Liver Dis 2015;47:797-804. [Crossref] [PubMed]
- Cubiella J, Vega P, Salve M, et al. Development and External Validation of a Faecal Immunochemical Test-Based Prediction Model for Colorectal Cancer Detection in Symptomatic Patients. BMC Med 2016;14:128. [Crossref] [PubMed]
- Cubiella J, Digby J, Rodríguez-Alonso L, et al. The Faecal Hemoglobin Concentration, Age and Sex Test Score: Development and External Validation of a Simple Prediction Tool for Colorectal Cancer Detection in Symptomatic Patients. Int J Cancer 2017;140:2201-11. [Crossref] [PubMed]
Cite this article as: Spiteri N, Skaife P. Get FIT for the new year: a review of the role of faecal immunochemical test for haemoglobin in patients with symptoms of colorectal disease. J Lab Precis Med 2018;3:52.


