
Adult hypoglycaemia; a narrative review on forensic aspects
Introduction
Forensic: “of, or used, in courts of law” [OED].
People with hypoglycaemia may be brought to the attention of the law for a variety of reasons. Most often it is due to the legitimate use of insulin leading to temporary brain malfunction, that is neuroglycopenia. This may result in misbehaviour and offences ranging from abusive language in a public place to murder—with petty crime and dangerous driving being the most common causes for court appearances. A more extensive and detailed account of hypoglycaemia as a defence against a criminal charge is available elsewhere (1). Rarely hypoglycaemia is a consequence of malicious (or accidental) administration of therapeutic insulin and it is with investigation of this type of hypoglycaemia that we intend to concentrate in this review.
Therapeutic insulin is not a single substance. Much prescribed insulin is still biosynthetic human or animal insulin but even more so are synthetic analogues with “insulin-like” properties, which may or may not be detected by immunoassays for human insulin. Therapeutic insulin—which includes insulin analogues—is marked with an * to distinguish it from human insulin whether endogenous or exogenous. Insulin measured by immunoassay is referred to as IRI and includes, in addition to human insulin, all animal, human and insulin analogues that are detected and semi-quantitated by immunoassay.
This short article reviews the literature regarding the pathophysiology of forensic hypoglycaemia in context of the criminal and clinical scenarios, and considers the role of the laboratory in contributing to the confirmation and elucidation of the aetiology of the hypoglycaemia. We present the following article in accordance with the Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/jlpm-20-104).
Hypoglycaemia as a defence against a criminal charge
Automatism due to hypoglycaemia is offered as a defence to otherwise criminal acts by patients with diabetes. It is, however, only tenable if the patient is receiving treatment with drugs that are capable of producing biochemical hypoglycaemia and not if their treatment is confined to diet or drugs, such as metformin, that do not produce hypoglycaemia.
Providing the evidence is sufficiently strong a plea of automatism is usually accepted by the court and the accused walks free (2,3).
Non-iatrogenic or spontaneous hypoglycaemia
In a tiny minority of cases spontaneous hypoglycaemia is claimed to be responsible for atypical and motiveless criminal behaviour.
While spontaneous hypoglycaemia causing automatism is a complete defence to a criminal charge it can only very rarely be substantiated. This is due to the rarity of spontaneous hypoglycaemia of sufficient severity to produce delinquent behaviour but also due to the difficulty of establishing it as the cause of the criminal act. This can only be done by measuring the accused person’s blood glucose concentration at the scene which is unlikely to occur in anything other than traffic offences and even then unusual (1).
Although hypoglycaemia due to insulinoma and other rare causes of fasting hypoglycaemia may lead to criminal behaviour (4), they do so exceedingly rarely and it is usually easily diagnosed providing the possibility is considered and investigated. Reactive hypoglycaemia, both idiopathic and secondary to bariatric surgery, is much more commonly offered as a defence and is generally much more difficult to prove.
In the past a diagnosis of reactive hypoglycaemia was usually made on a clinical history and the result of the long discredited “5-hour glucose tolerance test” or the only slightly less reliable “breakfast test”. These tests do not provide sufficient evidence that a suspect was suffering from hypoglycaemia at the time they were purported to have committed a criminal offence even though they were often accepted as doing so.
Nowadays, in addition to a self-delivered history of strange attacks consisting variously of “faintness”, anxiety, palpitations, sweatiness, and other symptoms associated with acute neuroglycopenia (5), evidence derived from ambulatory blood glucose monitoring, preferably with a continuous glucose monitoring device, should be required before a diagnosis of non-iatrogenic hypoglycaemia is seriously entertained (6). Evidence from a glucosidic meal test may be useful in suggesting the necessity for continuous glucose monitoring (5).
Hypoglycaemia as a criminal offence
Malicious hypoglycaemia is an extremely rare but important cause of unexplained hypoglycaemia. It takes many forms (Table 1) and the victim may be either dead or alive when first seen when they are usually referred to as a patient.
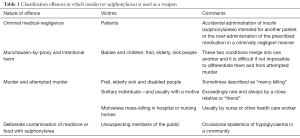
Full table
Establishing hypoglycaemia as the cause of the patient’s symptoms usually consisting of coma, but sometimes just confusion, is relatively easy, whereas establishing hypoglycaemia as the cause of death in someone found dead though possible may be extremely difficult.
Although the analytical techniques used to investigate hypoglycaemia in clinical and potentially forensic situations are the same, the data they generate are often more difficult to interpret. This is mainly because no reliable clinical history is available in the latter case.
A contemporaneous point of care test (POCT) glucose level below 3.0 mmol/L may serve as the first clue of hypoglycaemia in a patient suspected as being the victim of a crime; it should, however, never be accepted as the sufficient evidence to secure a conviction (1,3). This is especially true of purported victims of insulin poisoning because of the risk of POCT analytical error. It, nevertheless, provides an imperative reason for extensive investigation and is only likely to occur if every case of unexpected or unusual hypoglycaemia is considered potentially criminal and a venous sample of blood is collected immediately the diagnosis is made. This should be done before treatment with intravenous glucose is instituted and can be used later for laboratory analyses should it be necessary. This is especially true for elderly sick patients who develop hypoglycaemia in hospitals or nursing homes and which may be due to accidental administration of a hypoglycaemic drug intended for someone else, an uncommon response to their underlying illness or deliberate poisoning by malicious carers.
Treatment must not be delayed until confirmatory laboratory results become available but begin immediately after a pre-treatment blood sample has been collected. The brief interval between making a provisional diagnosis on the basis of the POCT and institution of treatment causes no adverse clinical consequence and the failure to collect the correct blood samples may have important consequences.
Treatment should commence with a bolus of 50% glucose followed by infusion of 10% glucose in amounts sufficient to maintain blood glucose within the range 5–12 mmol/L until the patient has recovered. A record should be kept of the total amount of glucose infused and, if suspicion of foul play remains after treatment has begun, analysis of the first sample of blood collected should be commenced—if it has not already been done!
Further investigations are the same as those for any other case of “spontaneous hypoglycaemia” but particular attention should be given to “chain of custody” of samples collected for analysis. Unless this is done the data obtained may be challenged and disregarded by some courts of law.
Interpretation of laboratory data
Patient alive when found
Interpretation of analytical results cannot be done without reference to the circumstances under which they were requested in forensic cases, any less than in clinical cases—however much the police or prosecuting authorities would like them to be. Every case of unexpected, unexplained hypoglycaemia sufficient to cause, or be associated with, severe symptoms is potentially suspicious and should be treated as such until proved otherwise.
A diagnosis of malicious hypoglycaemia is unlikely unless the venous blood glucose concentration is demonstrably below 2.5 mmol/L when the diagnosis of hypoglycaemia is first made. Although in the living patient, a solitary low unexplained POCT glucose result is sufficient reason to arouse suspicion and justify further investigation it is far from sufficient to establish a diagnosis of hypoglycaemia let alone one of malicious hypoglycaemia. In the past this was not so, and failure to understand this, led to erroneous diagnoses and unjustified convictions of nurses for murder especially of elderly sick hospital inpatients (7).
Glucose
A blood glucose concentration of greater than 2.5 mmol/L, though it may be associated with neuroglycopenic symptoms, is extremely unlikely to be due to malicious insulin administration; on the other hand no blood glucose concentration, however low, is proof that it was. The severity of the biochemical hypoglycaemia provides no evidence of malicious insulin use—blood glucose concentrations below 1.0 mmol/L may occur from a variety of conditions, including unrecognised sepsis and acute adrenal failure.
The amount of glucose intravenous needed to keep its blood concentration within the desired range of 5–10 mmol/L is similarly non-diagnostic. It may, however, provide some post-hoc evidence of malicious insulin administration if more than about 250 grams during the first 24 hours. Such large doses are sometimes required in non-insulin mediated hypoglycaemia in sick patients as well as in most cases of malicious insulin* or sulphonylurea overdose (1).
Insulin, C-peptide and proinsulin
Blood
Detection and measurement of insulin*, C-peptide and proinsulin is fundamental to the making of a diagnosis of malicious insulin administration. The three hormones should always be interpreted in context of each other, although insulin* is clearly the single most important—especially when analysed by liquid chromatography/mass-spectrometry (LC-MS) (8)—when identification of a non-prescribed insulin analogue is pathognomonic.
In the past immunoassay was the only method available for measuring insulin* and other peptides in cases of suspected homicide but relatively few investigators measured C-peptide with or without proinsulin along with insulin thereby reducing the diagnostic value of their test results as well as its inability to distinguish between it and its analogues. Although now this would be considered bad practice at best and negligent at worst, it was common in the past and reduced the value of the IRI results, however accurate they were. Although LC-MS has now replaced immunoassay as the definitive method for measuring insulin, C-peptide and proinsulin (9,10) especially in forensic investigations, immunoassay remains an indispensable screening procedure and remains perfectly adequate for most clinical work. It is still the only technique available for measuring these hormones in many communities.
There is no plasma IRI concentration that is diagnostic of felonious insulin administration: an inappropriately high plasma insulin (i.e., >100 pmol/L) and appropriately low C-peptide (<90 pmol/L), and/or proinsulin (<6 pmol/L) concentration, in the presence of a low blood glucose concentration is highly suggestive, as is a plasma C-peptide:insulin molar ratio of less than 1.0 regardless of the blood glucose concentration. In other words the C-peptide:insulin molar ratio can be useful even when glucose or glucagon has been given before the first (suspicious) blood sample was collected.
A similar pattern, of a higher insulin than C-peptide concentration, may also be seen in patients with the autoimmune insulin syndrome (AIS) (11,12) or the cause may never be found (13).
AIS has been offered as an explanation for elevated plasma or serum insulin:C-peptide ratios found in criminal cases. Apart from AIS being instantly recognisable by the presence of serum insulin auto-antibodies and despite having C-peptide:insulin molar ratios of <1.0 the plasma C-peptide levels are rarely less than 100 pmol/L in AIS whereas in insulin-induced hypoglycaemia they are invariably too low to measure.
In the cases of AIS in which the plasma concentration of both peptides were reported, C-peptide concentration averaged 10,394 (median: 5,000; range: 20–71,3000) pmol/L whereas in insulin-induced hypoglycaemia, except in patients with severe kidney disease, plasma C-peptide concentrations are invariably below the limit of detection. In AIS patients the average C-peptide:insulin ratio was 0.42, even exceeded a value of 1.0 (8.3%) in three cases. In malicious insulin-induced hypoglycaemia the plasma C-peptide:insulin ratio is less than 0.01, unless glucagon or intravenous glucose has already been given when it is still invariable less than 1.0.
Urine
Measurement of insulin in urine is of little diagnostic use as its concentration depends as heavily on kidney function as on its concentration in blood. Measurement of the urinary proinsulin:insulin molar ratio, on the other hand may turn out to be very useful for the diagnosis of homicidal insulin poisoning.
The normal molar ratio of proinsulin to insulin in urine is in the region of 0.14 and is elevated to 0.35 in patients with insulinoma (14) in whom plasma proinsulin levels are generally raised. It follows therefore, that in cases of exogenous hyperinsulinism in which plasma proinsulin levels are suppressed, the ratio of urinary proinsulin:insulin would be zero. At the time of this writing, however, the urinary proinsulin:insulin ratio has not been mentioned as providing valuable evidence in any court case.
The presence of intact molecules of insulin analogues or their metabolites by LC-MS is, however, pathognomonic when found in the urine of someone for whom they were not prescribed. It can be due to either accidental or malicious insulin* administration.
Other drugs
Sulphonylureas must always be excluded as the cause of unexplained hypoglycaemia. All three plasma pancreatic hormones levels are inappropriately high in sulphonylurea misuse thereby excluding exogenous insulin but not endogenous hyperinsulinism as the cause of a patient’s unexplained hypoglycaemia. Although a number of drugs and other substances, apart from those used to treat diabetes, also produce hypoglycaemia of sufficient severity to warrant hospital admission, they do so only sporadically and reports of death from this cause are rare. Their mode of action is varied and poorly understood but only rarely is (endogenous) insulin implicated.
A rigorous toxicological examination of both blood and urine is therefore indicated in any case of unexplained hypoglycaemia of sufficient severity to cause coma to ensure drug-induced hypoglycaemia is not overlooked.
Ketones: ß-hydroxybutyrate
Ketones can replace glucose as a source of energy in many tissues and do not require the presence of insulin to do so. They are traditionally measured in urine using Rothera’s reagents on a dip-stick. Their concentration in blood, as represented by ß-hydroxybutyrate (BHB), is not usually measured except in patients with diabetes but is helpful in distinguishing insulin-induced from most other types of hypoglycaemia. Its concentration is decreased to below 0.6 mmol/L in hypoglycaemia caused by insulin, insulin-like growth factors (IGF), extreme malnutrition and liver failure whereas in all other conditions causing hypoglycaemia its concentration is raised. Consequently, simple measurement of plasma BHB may provide an early clue to the correct diagnosis and remove the necessity for suspicion in the vast majority of cases of unexplained hypoglycaemia.
Lactate
Lactate is the product of the anaerobic breakdown of glucose and is normally present in the blood at a concentration below 1.8 mmol/L. Its concentration increases when there is hypoxia or poor perfusion of tissues. A raised concentration of lactate in the blood is therefore indicative of a number of disorders many of which, such as sepsis, liver disease or heart failure, can also cause hypoglycaemia. Malicious insulin usage is not associated with hyperlactataemia and its finding, therefore, should arouse suspicion that some other cause might have been responsible for the patient’s hypoglycaemia.
The measurement of lactate in post mortem blood and especially vitreous humour may be helpful in confirming or dismissing a diagnosis of suspected death from hypoglycaemia as discussed below.
Alcohol
Alcohol is one of the commonest causes of spontaneous hypoglycaemia in patients admitted to hospital and its measurement in any case of unexplained hypoglycaemia is essential. The concentration of alcohol need not be very high to provide evidence of causation since it is possible to back-calculate the pre-morbid concentration as long as the interval since the last drink is known.
Routine tests for ketones using Rothera’s reagents, whether applied to urine or blood, often yield negative results since they fail to detect ß-hydroxybutyrate, the main ketone raised in alcohol induced hypoglycaemia.
Potassium
Plasma potassium is often subnormal in patients with hypoglycaemia whatever the cause. It is invariably below 4.0 mmol/L in those who have attempted suicide with insulin (1), and its measurement may therefore be useful in ruling out homicidal insulin administration in cases of unexplained hypoglycaemia in which blood insulin measurements were not made at the relevant time. While an initial plasma potassium concentration below 4.0 mmol/L provides no evidence of it causation one above 4.0 mmol/L makes a diagnosis of malicious insulin induced hypoglycaemia unlikely.
Victim found dead
Murder or manslaughter, using insulin* as the weapon, is extremely rare. Unless suspected, however, in every case of unexplained death it is likely to go undetected. Conversely, the long interval between a person receiving a lethal dose of insulin and their demise ensures that the victim will often be found in the comatose state that precedes death and be saved or left seriously brain damaged (15).
This is especially the case in people who attempt suicide with insulin which is the commonest cause of death from malicious insulin use. In both suicide and non-suicide cases the victim is often someone who is diabetic or is a close relative or friend with easy access to insulin*, but occasionally it is someone who has obtained it illicitly. Murder using insulin as a weapon by someone unknown to the victim is virtually unknown except in cases of mass or so-called “mercy” killing by one or more health-care workers in a hospital or nursing home environment (16,17).
Investigation of the cause of death by insulin* is the same for murder as for suicide but in the latter there are often clues to the cause at or near the scene. A minority of suicides, however, go to great lengths to hide the cause of their death. The interval between the injection and its taking effect—usually between 10 and 30 minutes—is sufficient to enable them to dispose of the evidence. As a result, realisation that a person’s death was due to suicide or murder using insulin as the weapon may be delayed for so long that realistic laboratory investigation of the cause has disappeared.
Typically there are no morphological features that identify a corpse as due to insulin poisoning. A thorough search of the body may reveal the site of one or more injection sites (18), but these may be obscured by being in such unlikely sites as the scrotum or vagina that are easy to get to but difficult to find. If a site is identified then a generous sample of the surrounding tissue should be excised at autopsy and sent for immuno-histological examination and chemical analysis for insulin*.
Samples of venous blood from a peripheral blood vessel, CSF, vitreous humour from both eyes and urine should be collected for later analysis in the laboratory. Blood must be separated immediately and the serum frozen and kept at –200 °C until analysed for insulin, C-peptide and proinsulin. Haemolysed blood is very unlikely to yield positive results when assayed by immunoassay (19), but may contain fragments of insulin analogues that are recognised by LC-MS.
Glucose
Glucose disappears from blood so rapidly after death that its measurement is of very little value unless undertaken within 1 or 2 hours of death—which is unlikely to occur in practice. Measurements carried out later may be seriously misleading, especially if undertaken on cardiac or central venous blood serum when they may be abnormally high, even in cases of proven insulin* induced hypoglycaemic death. This is due to post-mortem diffusion of glucose from the liver into surrounding tissues and blood.
Glucose also disappears from vitreous humour after death, contrary to what was once thought and still believed by some pathologists. Nevertheless, a vitreous glucose concentration of less than 1 mmol/L may provide the first clue to an unsuspected insulin-induced death. Even such low concentrations are, however, very weak evidence on their own of ante mortem hypoglycaemia and are only slightly improved by combining its measurement with that of lactate in the so-called Traub formula. A combined glucose and lactate (Traub) concentration of less than 3 mmol/L indicates ante mortem hypoglycaemia regardless of cause and always warrants further investigation. A Traub concentration of more than 7 mmol/L effectively rules out the diagnosis of death from hypoglycaemia.
Insulin, C-peptide and proinsulin
All three peptides disappear from the blood after death and unless samples are collected from a peripheral vein within 24–48 hours of death are unlikely to yield meaningful results. This is in part due to the inevitable post mortem haemolysis (18), and partly to enzymatic degradation. Blood collected from the heart or inferior vena cava may be contaminated by insulin diffusing out of the pancreatic islets and so is next to useless for analysis by immunoassay but may reveal the presence of an unauthorised insulin analogue when analysed by LC-MS. Although haemolysed serum is unsuitable for immunoassay, it may be suitable when analysed by LC-MS for identifying fragments of insulin analogues which should not have been there.
The absence of insulin* from non-haemolysed post-mortem blood serum, collected within 24–48 hours of death makes homicide, either suicidal or murderous, unlikely but not impossible. In the relatively few cases reported in the literature in which a valid measurement was made in post-mortem, serum IRI concentrations ranged from 50–10,000 pmol/L—the higher levels invariable being reported in suicides. Although insulin* is only rarely detected in peripheral blood more than 48 hours after death it remains for longer at the injection site, if one can be identified, and may be detected by immunohistology or preferably by chemical analysis. How long insulin may be present at an injection site post mortem is unknown but it is unlikely that claims that it is still detectable in putrefying exhumed bodies, 6 or more months after burial, will be substantiated by chemical analysis—the sine qua non for diagnosis.
Serum C-peptide measurements from victims of malicious insulin administration are rare but those that have been made are invariably low. Measurements of proinsulin are even rarer and have not contributed to the diagnosis.
The measurement of insulin in vitreous humour is comparative new but has already established itself as the preferred test for identification of suicidal/homicidal insulin misuse. It has the advantage that no haemolysis is possible though proteolysis continues. Consequently, though insulin levels are normally much lower than in blood they decline more slowly after death and therefore may be measured and identified many days post mortem.
In non-diabetic persons, both ante mortem and post mortem vitreous IRI levels are invariably below 10 pmol/L and usually immeasurably low; somewhat surprisingly levels greater than this, but below 20 pmol/L are sometimes found in diabetic patients on insulin therapy (20,21). The mean concentration of insulin* in vitreous in the 11 patients in whom it is known to have been measured, and to have died from insulin poisoning, was 28 pmol/L; range: <10–618 pmol/L; median: 150 pmol/L. The one patient in whom vitreous insulin* was undetectable had survived 10 days before dying.
Immunohistology
Insulin persists at its site of injection for periods of several days depending on its formulation and dosage. The former is especially important when the dosage is small but with the bigger doses encountered in most suicides even rapidly acting formulations may persist for several days. Exactly how long maliciously administered insulin remains detectable after death is a moot point and depends both upon how long the victim survived before dying and how great time elapsed between death and the post-mortem and whether the corpse was chilled or frozen (22). Most authorities have concluded that no insulin remains at an injection site if the post-mortem is delayed beyond about 10 days.
Immunohistological examination for insulin of tissue removed from around the site of a suspicious injection site is often rewarding (23). It should not, however, be accepted as irrefutable evidence of malicious insulin misuse in a corpse unless confirmed by chemical analysis of a tissue extract. Identification of the insulin type by LC-MS is a bonus (10).
Reports of immune histochemical identification of insulin in exhumed corpses, many months after death, and after putrefaction has set-in, are barely credible and immune histochemical diagnosis of insulin homicide is unacceptable as evidence of malicious insulin usage in a corpse more than 1 month after death unless supported by incontrovertible chemical evidence (10,24).
Neuropathology
The brain is the only organ anatomically damaged by prolonged hypoglycaemia. Its detailed anatomical and histological examination is therefore an integral part of a suspected death from malicious insulin use. The whole brain should be preserved intact before being subject to examination by a neuropathologist. While there is evidence to suggest that some of the anatomical damage observed in hypoglycaemic deaths is due to attempts at too rapid restoration of normoglycaemia (25), there are some changes that are believed to be produced by hypoglycaemia per se. There is, however, still considerable debate as to whether neuropathological changes in the brain produced by hypoglycaemia are sufficiently distinct from those produced by hypoxia to be certain of securing a conviction in cases where supporting biochemical evidence is lacking.
The regions of the brain that are affected most are the cerebral cortex and the hippocampus but authorities differ as to whether any of the changes are diagnostic. The brain stem is usually preserved which helps explain the persistent vegetative state of those who survive malicious insulin use after prolonged but unsuccessful treatment of their hypoglycaemic state.
Suicide with insulin or sulponylurea
The study of insulin suicides, and more especially of failed suicides (26), has provided much of the information about the forensic toxicology of insulin but much remains to be learned. Suicide always involves a coroner and usually an inquest takes place at which expert advice may be sought.
Suicide, and more commonly its attempt, is no longer a crime in most jurisdictions in the world but still carries opprobrium and shame in many communities. It may also jeopardize life insurance and other civil contracts. Insulin*+ as a suicidal agent may not only be used by patients with diabetes, their close relatives and friends but also those without any known connection with diabetes who access it either legally or illegally.
It is important in diabetic patients to distinguish suicide with insulin* from accidental death due to its legitimate use. This is usually extremely easy due to clues such as a suicide note or a collection of insulin vials by their bedside; it may also be extremely difficult. A post mortem insulin* measurement on post-mortem blood, but especially of vitreous humour, may help resolve the issue, especially if carried out within 24–48 hours of death. Caution in interpretation of the results is however required especially if immunoassay rather than LC-MS is used.
In at least one case known to the authors a misdiagnosis of suicide rather than accidental death was only averted when one of the authors (VM) pointed out to the coroner that the unexpectedly high post-mortem serum IRI level was due to therapeutic use of levermir rather than to suicidal overdosing with insulin. With the introduction of LC-MS measurements for insulin in all forensic cases such errors are unlikely to occur.
Unlike most toxic substances—which are taken by mouth—the concentration of insulin in the blood of a patient, whether alive or deceased, is a poor indicator of the amount of the drug administered. More informative is the dose and duration of intravenous glucose administration to prevent relapse—providing insulin is known from biochemical analysis to be the cause of the patient’s hypoglycaemia. With accidental over-dosage the amount required is always small (less than 50 grams) and of short duration (less than 6 hours) whereas in deliberate or malicious administration the glucose dose is bigger and the duration longer.
The average requirement of glucose till full recovery may be anywhere between 160 and 1,100 g and the duration of treatment might vary from 12 to 62 hours or more. This has led to the misconception that the requirement for large, continuous infusions of glucose to prevent relapse into hypoglycaemia is invariably due to malicious insulin administration, even when there was no direct evidence of insulin involvement. As a result, there have been wrongful convictions for murder (7). Similar needs for glucose are occasionally seen in non-insulin mediated spontaneous hypoglycaemia (1).
Clustered hypoglycaemia
Clustered hypoglycaemia, the occurrence of three or more cases of unexpected hypoglycaemia, in a confined environment within a short period of one another, may be spontaneous or malicious in origin. The earliest clusters recorded were due to the ingestion of natural toxins such as toxic mushrooms and unripe Akee nuts. Other clusters have been due to accidental or deliberate contamination of medicinal drugs with sulphonylureas and due to deliberate poisoning of patients with insulin in hospitals and care homes. Deliberate poisoning of patients presents a number of problems including establishing the perpetrator and determining, in retrospect, which patients who died with hypoglycaemia were due to poisoning and which were due to natural causes. It is upon such unreliable information that jurists must often make life-changing decisions.
The role of the expert witness
The role of the expert witness is to assist the court regardless of whether they are called by the prosecution or defence. They are there to help the court understand the complexity of hypoglycaemia: what it is, how it was caused in this particular case and its likely effect on the victim or defendant, depending on the nature of the case. They are not there primarily to describe evidence that they themselves have elicited—although they may do so—since that is the role of the so-called “professional” witnesses.
Experts in the forensic aspects, as opposed to clinical practice, of hypoglycaemia are drawn from several disciplines including toxicology, endocrinology, forensic pathology and clinical biochemistry—possibly the most important of all. Whatever the expert’s primary discipline their written report should be the same regardless of which team they may have consulted with as a medico-scientific advisor prior to trial.
In the case of a defendant charged with a criminal offence the experts would be expected to express an opinion on whether the subject did or not suffer from neuroglycopenia of sufficient severity to cause temporary incapacity to commission a crime; in other words to behave as an automaton.
In cases where insulin is suspected of being used as an offensive weapon the expert would be expected to demonstrate to the court that it was or that it was not used in this way. They should not venture an opinion on who was or might have been responsible. Nor should they, in cross examination, allow themselves to stray from their particular area of expertise as has been known to happen and admitting to ignorance in response to a question is both more honourable and legally correct than attempting to bluff.
Exactly who qualifies as an expert is a moot point there is no generally accepted definition. All should enjoy high regard in their primary profession; some will belong to the Academy of Experts—a body widely respected by the judiciary others to the Society of Expert Witnesses—a professional association of those accustomed to giving expert advice in court—but most will just be knowledgeable about the subject of their expertise in this case hypoglycaemia.
Anyone whose expertise is unchallenged can describe themselves as an expert and what they have to say will be taken into account in the judge’s summing up. It is therefore the responsibility of the opposing legal team—guided by their own experts—to expose any shortcomings in the expertise of any purported expert called by the other side. The ability to do this well and without incurring the wrath of the court is the skill of advocacy—not of an expert witness!
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Laboratory and Precision Medicine for the series “Adult Spontaneous Hypoglycaemia”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/jlpm-20-104
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jlpm-20-104). The series “Adult Spontaneous Hypoglycaemia” was commissioned by the editorial office without any funding or sponsorship. RG serves as an unpaid Guest Editor of the series and serves as an unpaid editorial board member of Journal of Laboratory and Precision Medicine from March 2020 to March 2022. The other author has no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Marks V. Forensic Aspects of Hypoglycaemia. Boca Raton CRC Press 2019:1-375.
- Frier BM. Hypoglycaemia and criminal responsibility. In: Andreani D, Marks V, Lefebvre PJ. editors. Hypoglycemia. Serono Symposia Publications. New York: Raven Press, 1987:201-9.
- Marks V. Hypoglycaemia and automatism. Med Sci Law 2015;55:186-93. [Crossref] [PubMed]
- Marks V. Hypoglycaemia--real and unreal, lawful and unlawful: the 1994 Banting Lecture. Diabet Med 1995;12:850-64. [Crossref] [PubMed]
- Brun JF, Fedou C, Mercier J. Postprandial reactive hypoglycemia. Diabetes Metab 2000;26:337-51. [PubMed]
- Mongraw-Chaffin M, Beavers DP, McClain DA. Hypoglycemic symptoms in the absence of diabetes: pilot evidence of clinical hypoglycemia in young women. J Clin Transl Endocrinol 2019;18:100202 [Crossref] [PubMed]
- Inside Justice. A Jury blinded by Science: the case of Colin Noris. Southampton: Botley Mills, 2013.
- Thevis M, Thomas A, Delahaut P, et al. Qualitative determination of synthetic analogues of insulin in human plasma by immunoaffinity purification and liquid chromatography-tandem mass spectrometry for doping control purposes. Anal Chem 2005;77:3579-85. [Crossref] [PubMed]
- Hess C, Madea B, Daldrup T, et al. Determination of hypoglycaemia induced by insulin or its synthetic analogues post mortem. Drug Test Anal 2013;5:802-7. [Crossref] [PubMed]
- Legg KM, Labay LM, Aiken SS, et al. Validation of a fully automated immunoaffinity workflow for the detection and quantification of insulin analogs by LC-MS-MS in postmortem vitreous humor. J Anal Toxicol 2019;43:505-11. [Crossref] [PubMed]
- Hirata Y. Autoimmune insulin syndrome “up to date”. In: Andreani D, Marks V, Lefebvre PJ. editors. Hypoglycemia. Serono Symposia Publications. New York: Raven Press, 1987:105-18.
- Church D, Cardoso L, Bradbury S, et al. Diagnosis of insulin autoimmune syndrome using polyethylene glycol precipitation and gel filtration chromatography with ex vivo insulin exchange. Clin Endocrinol (Oxf) 2017;86:347-53. [Crossref] [PubMed]
- Villaume C, Dollet JM, Beck B, et al. Hyperinsulinemia associated with normal C-peptide levels in a woman treated with isoniazide. Biomed Pharmacother 1982;36:32-5. [PubMed]
- Constan L, Mako M, Juhn D, et al. The excretion of proinsulin and insulin in urine. Diabetologia 1975;11:119-23. [Crossref] [PubMed]
- Barbara G, Mégarbane B, Argaud L, et al. Functional outcome of patients with prolonged hypoglycemic encephalopathy. Ann Intensive Care 2017;7:54. [Crossref] [PubMed]
- Yorker BC, Kizer KW, Lampe P, et al. Serial murder by healthcare professionals. J Forensic Sci 2006;51:1362-71. [Crossref] [PubMed]
- Field J, Pearson A. Caring to death: the murder of patients by nurses. Int J Nurs Pract 2010;16:301-9. [Crossref] [PubMed]
- Birkinshaw VJ, Gurd MR, Randall SS, et al. Investigations in a case of murder by insulin poisoning. Br Med J 1958;2:463-8. [Crossref] [PubMed]
- Wunder C, Kauert GF, Toennes SW. Factors leading to the degradation/loss of insulin in postmortem blood samples. Forensic Sci Int 2014;241:173-7. [Crossref] [PubMed]
- Palmiere C, Sabatasso S, Torrent C, et al. Post-mortem determination of insulin using chemiluminescence enzyme immunoassay: preliminary results. Drug Test Anal 2015;7:797-803. [Crossref] [PubMed]
- Sahajpal NS, Jain S, Vig V, et al. Insulin in the vitreous humor of patients with proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci 2018;59:abstr 5366.
- Tong F, Wu R, Huang W, et al. Forensic aspects of homicides by insulin overdose. Forensic Sci Int 2017;278:9-15. [Crossref] [PubMed]
- Lutz R, Pedal I, Wetzel C, et al. Insulin injection sites: morphology and immunohistochemistry. Forensic Sci Int 1997;90:93-101. [Crossref] [PubMed]
- Heyndrickx A, Van Peteghem C, Van den Heede M, et al. Insulin murders: isolation and identification by radio-immunoassay after several months of inhumation. In: Oliver JS. editor. Forensic toxicology. Boston: Springer, 1980:48-57.
- Suh SW, Gum ET, Hamby AM, et al. Hypoglycemic neuronal death is triggered by glucose reperfusion and activation of neuronal NADPH oxidase. J Clin Invest 2007;117:910-8. [Crossref] [PubMed]
- Mégarbane B, Deye N, Bloch V, et al. Intentional overdose with insulin: prognostic factors and toxicokinetic/toxicodynamic profiles. Crit Care 2007;11:R115. [Crossref] [PubMed]
Cite this article as: Marks V, Gama R. Adult hypoglycaemia; a narrative review on forensic aspects. J Lab Precis Med 2021;6:11.


