
Potential drawbacks of pharmacy-based COVID-19 testing
In a recent article, Risanger and colleagues have underpinned the potential benefits of establishing a pharmacy-based model of rapid diagnostic testing for coronavirus disease 2019 (COVD-19) (1). Although increasing and optimizing the access to diagnostic testing is a cornerstone in prevention and management of the ongoing severe acute respiratory disease coronavirus 2 (SARS-CoV-2) pandemic outbreak, we would like to briefly highlight some important caveats that may afflict a pharmacy-based strategy for replacing or supporting conventional laboratory-based SARS-CoV-2 diagnostic testing (2).
The first aspect that needs to be highlighted, is that specimen self-collection by patients themselves does not provide the same diagnostic performance as collection by healthcare personnel, especially when patients have not been appropriately trained. Evidence of this has been provided in several studies, including that published by McCulloch et al. (3), who concluded that patient-collected nasopharyngeal swabs had 20% lower diagnostic sensitivity compared to clinician-collected specimens, especially when the viral load is low, but still clinically significant in terms of potential inter-human transmission. Similar results were reported by Tan et al. (4), who also showed that self-collection may be characterized by nearly 30% lower diagnostic sensitivity compared to collection by healthcare worker for specimens with cycle thresholds higher than 30. As there is now widespread literature highlighting the potential limitations (especially with respect to false negative test results) of self-collecting nasopharyngeal swabs (5), serious doubts remain as to the accuracy of this practice.
A second aspect that needs to be highlighted is the testing technology used for diagnosing both symptomatic and (especially) asymptomatic COVID-19 infections. Rapid point of care (POC) molecular or antigenic assays do not provide comparable diagnostic performance as routine, laboratory-based, test, as clearly highlighted by the Cochrane COVID-19 Diagnostic Test Accuracy Group (6). In particular, rapid POC tests are still currently characterized by poor diagnostic sensitivity in identifying COVID-19 patients with low viral load (between 34–100% for rapid molecular tests and between 8–70% for rapid antigen tests, respectively), who are however important vehicles of viral transmission, accounting for nearly one-fourth of all documented asymptomatic contagions (7).
Insufficient quality assurance throughout the total POC testing process is another potential limitation (8).An international external quality assessment survey carried out for purpose of reviewing the quality of SARS-CoV-2 molecular detection has evidenced a considerably high coefficient of variation (i.e., between 35–54%) in terms of cycle threshold reporting across different clinical specimens (9). Thus, lack of establishing rigorous quality assessment schemes in all pharmacies providing COVID-19 diagnostics could end up generating poorly comparable or even unreliable data. Strict laboratory supervision of all decentralized testing practices, from test selection to results reporting, is unavoidable. On the other hand, resorting alternative strategies such as self-collected salivary samples (which allow less invasive and minimized hazard exposure) connected with molecular or laboratory-based antigen assays using high-sensitive chemiluminescent tracers, can be eventually envisaged for assuring better access to testing, while preserving adequate quality and reliability (10).
A final concern relates to the need of receiving expert counselling on accuracy and clinical implications of this type of testing. This importance of this activity, which cannot be always offered outside the boundaries of laboratory medicine services, has been recently emphasized in an editorial published by Mahase (11). Basically, full information on risks and benefits shall be offered to all those undergoing decentralized COVID-19 rapid diagnostics. Reinforced recommendations shall then be supplied that negative test results do not definitely exclude active SARS-CoV-2 infection, nor shall give false sense of security that allows adopting permissive behaviours or ignorance of restrictions, especially when living with fragile or more vulnerable individuals.
As the cost-effectiveness and reliability of mass population screening remains to be proven, especially when involving asymptomatic individuals and supported by insufficiently sensitive techniques (12), we proffer that pharmacy-based testing may currently carry more drawbacks than advantages to be considered a reliable strategy, as summarized in Table 1. Careful consideration of specimen collection and handling procedures, diagnostic accuracy of testing technologies, quality assurance programs, expert counselling and cost-effectiveness analysis must be considered priorities in any pharmacy-based testing strategy.
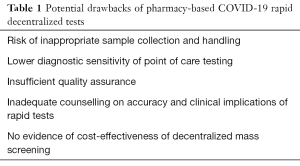
Full table
Notably, the authors of a recent Cochrane rapid review have concluded that universal screening, especially based on rapid laboratory tests, has a “very low” sensitivity and thereby carries a relevant risk of missing a high proportion of infected individuals, thus fostering virus spread (13). On the other hand, the “low” specificity of these techniques may also lead to falsely labelling some healthy subjects as positive, who will then require additional (and virtually unnecessary) confirmatory laboratory testing or will be needlessly forced to respect strengthened individual restrictions (13). In keeping with these concepts, we thoughtfully endorse the conclusion of Gray and colleagues, that no mass testing may be much better than bad testing (14).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jlpm-21-10). GL serves as an unpaid Editor-in-Chief of the Journal of Laboratory and Precision Medicine from November 2016 to October 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Risanger S, Singh B, Morton D, et al. Selecting pharmacies for COVID-19 testing to ensure access. Health Care Manag Sci 2021; [Crossref] [PubMed]
- Lippi G, Mattiuzzi C, Bovo C, et al. Current laboratory diagnostics of coronavirus disease 2019 (COVID-19). Acta Biomed 2020;91:137-45. [PubMed]
- McCulloch DJ, Kim AE, Wilcox NC, et al. Comparison of Unsupervised Home Self-collected Midnasal Swabs With Clinician-Collected Nasopharyngeal Swabs for Detection of SARS-CoV-2 Infection. JAMA Netw Open 2020;3:e2016382 [Crossref] [PubMed]
- Tan SY, Tey HL, Lim ETH, et al. The accuracy of healthcare worker versus self collected (2-in-1) Oropharyngeal and Bilateral Mid-Turbinate (OPMT) swabs and saliva samples for SARS-CoV-2. PLoS One 2020;15:e0244417 [Crossref] [PubMed]
- Kinloch NN, Ritchie G, Brumme CJ, et al. Suboptimal Biological Sampling as a Probable Cause of False-Negative COVID-19 Diagnostic Test Results. J Infect Dis 2020;222:899-902. [Crossref] [PubMed]
- Dinnes J, Deeks JJ, Adriano A, et al. Rapid, point-of-care antigen and molecular-based tests for diagnosis of SARS-CoV-2 infection. Cochrane Database Syst Rev 2020;8:CD013705 [PubMed]
- Johansson MA, Quandelacy TM, Kada S, et al. SARS-CoV-2 Transmission From People Without COVID-19 Symptoms. JAMA Netw Open 2021;4:e2035057 [Crossref] [PubMed]
- Riccò M, Ferraro P, Gualerzi G, et al. Point-of-Care Diagnostic Tests for Detecting SARS-CoV-2 Antibodies: A Systematic Review and Meta-Analysis of Real-World Data. J Clin Med 2020;9:1515. [Crossref] [PubMed]
- Matheeussen V, Corman VM, Donoso Mantke O, et al. International external quality assessment for SARS-CoV-2 molecular detection and survey on clinical laboratory preparedness during the COVID-19 pandemic, April/May 2020. Euro Surveill 2020;25:2001223 [Crossref] [PubMed]
- Basso D, Aita A, Padoan A, et al. Salivary SARS-CoV-2 antigen rapid detection: A prospective cohort study. Clin Chim Acta 2021;517:54-9. [Crossref] [PubMed]
- Mahase E. Covid-19: People are not being warned about pitfalls of mass testing. BMJ 2021;372: [PubMed]
- Lippi G, Henry BM, Sanchis-Gomar F. Potential drawbacks of frequent asymptomatic coronavirus disease 2019 (COVID-19) testing. Infect Control Hosp Epidemiol 2020; [Crossref] [PubMed]
- Viswanathan M, Kahwati L, Jahn B, et al. Universal screening for SARS-CoV-2 infection: a rapid review. Cochrane Database Syst Rev 2020;9:CD013718 [PubMed]
- Gray N, Calleja D, Wimbush A, et al. Is "no test is better than a bad test"? Impact of diagnostic uncertainty in mass testing on the spread of COVID-19. PLoS One 2020;15:e0240775 Erratum in: PLoS One 2021;16:e0247129. [Crossref] [PubMed]
Cite this article as: Lippi G, Henry BM, Plebani M. Potential drawbacks of pharmacy-based COVID-19 testing. J Lab Precis Med 2021;6:10.


