
Standardisation of adjusted calcium equation: the UK approach—a narrative review
Introduction
The estimation of calcium in serum has proved to be one of the most informative tests in clinical biochemistry. The effect of binding of calcium to albumin (and to other proteins and serum constituents to some extent) has made interpretation difficult in some circumstances. Some 50 years ago the concept of adjusting serum calcium levels to compensate for low or high albumin values was proposed. The aim was to provide an estimate of the patient’s calcium level were their albumin to be normal, and thus to improve laboratory reporting of individual patients’ physiological calcium status. More recently, in the UK, there have been several standard protocols proposed to encourage generation of local adjustment equations. The performance of these adjustment equations has been questioned, particularly in the context of other pathology. Increasing use of ionised calcium estimations, often within a point-of-care testing (POCT) panel, has raised the question of the future utility of calcium adjustment.
This article reviews (I) the development of calcium adjustment equations in the UK over the last 50 years and initiatives to improve and standardise methodology; (II) the assessment of response to the standardisation initiatives. This is followed by discussion of the possible shortcomings of the mechanics and validation of a standard approach for generation of local adjustment equations. Various solutions for sub-optimal performance of the adjustment equations in patients with pathologies which are likely to affect the binding of calcium to albumin are explored. The use of ionised calcium measurements as an alternative option in certain pathologies is considered. We present the following article in accordance with the Narrative Review reporting checklist (available at https://jlpm.amegroups.com/article/view/10.21037/jlpm-22-35/rc).
Methods
Papers included in this review were identified using the Google Scholar search engine using the search terms: adjusted calcium; ionised calcium; albumin estimation in serum. The search timeframe was from the first documented use of albumin for calcium adjustment in 1973 until 2022. All published case reports, studies and literature reviews worldwide, in English, were considered in producing this article. Table 1 shows the detailed search strategy.
Table 1
| Item | Specification |
|---|---|
| Database searched | Google Scholar |
| Timeframe of search | 1973–2022 (May) |
| Search terms used (including Boolean operators) | (I) Calcium AND adjusted |
| (II) Calcium AND ionised OR ionized | |
| (III) Albumin AND serum AND estimated OR estimation OR measured OR measurement | |
| Limitations of search | Limited to the title of the articles |
| Any additional considerations | Some papers were identified by reviewing reference lists of relevant publications |
Evolution of calcium adjustment
The evolution of adjusted serum calcium in the UK has followed a somewhat erratic path. In 1973, Payne et al. (1) proposed that adjustment of serum calcium should be based on correlation with albumin rather than total protein or specific gravity. Interestingly, the mechanism for derivation of the adjustment equation involved correction to the mean of the quoted “normal range” of the total calcium assay in the laboratory at the time, thus representing the first attempt to normalise the adjustment. Over the following decade the utility of calcium adjustment was confirmed (2) and the use of a simple adjustment equation derived from the original data and further validated by the authors, was promoted: adjusted calcium (mmol/L) = measured calcium (mmol/L) + [40 – albumin (g/L)] × 0.025.
This simple equation [published at a time before the extensive implementation of Laboratory Information Management Systems (LIMS)] allowed an ad hoc adjustment of actual calcium values in order to confirm or refute abnormal calcium homeostasis. Thus, the equation (with 0.025 subsequently rounded down to 0.02) became extensively used in laboratories, and entrenched in the UK as a reliable universal equation for all methods despite the authors’ original caveats to the contrary.
By the late 1980s, LIMS generated data were becoming more commonly available as well as computerised statistical packages. This prompted reappraisal of the validity of any universal equation (3) and encouraged the use of regression equations based on local data (4,5) otherwise the risk of misclassification of borderline hypo- or hypercalcaemic patients would be considerable. The availability of databases of thousands of patient results enabled more detailed investigation of the adjustment concept. Various limitations were exposed and the universal application of adjustment to all patient results and to certain disease groups was questioned (6). At the same time, the accuracy of routine laboratory methods for the estimation of both albumin and calcium were under scrutiny (7).
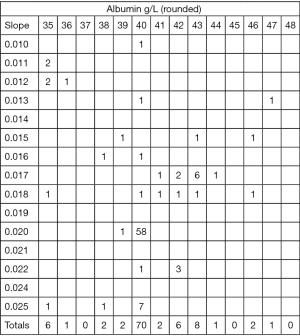
By the turn of the millennium, it was evident that there was a lack of strategic intent in relation to the use of calcium adjustment: many laboratories were not adjusting calcium routinely, and those that were had many different approaches. The situation was not systematically audited until 2008 when both Wales External Quality Assessment Scheme (WEQAS) and the Keele Benchmarking Project collected information on the current adjustment equations in use. Figure 1 shows a summary of that data. The number of different equations in use is scientifically consistent with the number of different methods in use, but what is surprising is that of 101 laboratories who provided data 58 were using the original adjustment proposed by Payne et al. (2) in 1979, despite ample evidence that it was unsuitable for universal application.
In 2007, the Pathology Harmony initiative was established in Birmingham. The aim was to examine the variation in reference ranges and units quoted by UK laboratories for commonly measured analytes and where the underlying science did not convincingly explain identified variation, to recommend harmonised ranges for use throughout the UK (8). In November 2007, a national meeting was held which ratified proposals for over 30 test reference ranges and units to be adopted for universal use. Phase 2 of Pathology Harmony, which commenced in 2008 considered a further group of analytes including serum calcium. When looking at reference ranges for calcium quoted by laboratories contributing to the project in combination with evidence from external quality assurance (EQA) data of bias and variation in the analytical methods in use it was deemed inappropriate to propose a harmonised range for serum calcium at that time. However, an alternative proposal to harmonise adjusted calcium was tabled. This would require laboratories to derive local adjustment equations and normalise these to a mean calcium of 2.4 mmol/L with a harmonised reference range of 2.20–2.60 mmol/L. At the Phase 2 Review Meeting held in November 2009 this proposal was accepted and became part of the subsequent recommendations (9).
In 2015, the Association for Clinical Biochemistry and Laboratory Medicine (ACB) published a position paper on albumin-adjusted calcium (10). The recommendations supported the need for a harmonised approach and emphasised that laboratories should derive local adjustment equations. Further detailed advice on generating a locally derived equation was included to result in an equation in the form:
The substitution of 2.4 mmol/L for the mean total calcium (as the mid-point of the healthy population calcium reference range) was suggested; this would result in the equation proposed by Pathology Harmony:
The substitution of 2.4 mmol/L was not mandated, presumably in order to allow laboratories with mid-point of reference range value significantly different from 2.4 to substitute that value instead together with their own appropriate reference range—a point that was perhaps not sufficiently clarified.
Since 2015, work has been done to further investigate the validity of this approach especially in various sub-groups of patients based on disease, age, etc. and these have revealed various shortcomings which may result in inaccurate adjustment in certain circumstances. The possibility of variants of the equation for certain patient cohorts may be considered in future (11).
In the meantime, the essential requirement is to undertake further surveys of UK labs to demonstrate whether the standardisation initiatives described have resulted in better outcomes and a more unified approach for clinicians.
Proposed method for serum calcium adjustment
The Pathology Harmony Group proposed the use of locally derived adjustment equations by collecting data from the laboratories’ information systems using a procedure based on that described by Barth et al. (4). A very similar approach is also recommended by the ACB position paper (10).
- Collect recent data from the LIMS to generate at least 1,000 adult patient values for total calcium and albumin using the following sifting criteria (setting the data gather to include only one result per patient):
- Urea <15 mmol/L;
- Creatinine <200 mmol/L;
- Potassium >3.5 and <5.5 mmol/L;
- Calcium >2.0 and <2.7 mmol/L;
- Alkaline phosphatase (ALP) and alanine aminotransferase (ALT) [or aspartate aminotransferase (AST)] within laboratory reference range;
- Parathyroid hormone (PTH), if measured, within reference range.
- Exclude patients attending the departments of haematology, endocrinology, oncology, nephrology; also patients from intensive care, critical care, and renal dialysis units.
- Examine the collected data for adequate spread; they should include values for albumin from the manufacturer’s lower detection limit for albumin up to about 55 g/L. Ideally there should be at least 30 data points for each integral albumin value from 20 to 50 g/L although this may not always be possible at the limits.
- Calculate the least squares regression of calcium on albumin using a standard statistical package.
- Subtract the intercept on the y-axis of the line of best fit from 2.4, and substitute this value into the adjustment equation in the general form:
where x is the slope of the regression line and y the intercept subtracted from 2.4.
In order to validate the equation two procedures were recommended:
First, the newly derived adjustment equation should be applied to the collected data.
Calculate the mean and standard deviation of the adjusted calcium values. Using appropriate statistical method (depending on data distribution), calculate the 95% limits, either as mean ± 2 standard deviation (SD) or as the 2.5th and 97.5th percentiles using a non-parametric method.
The mean should be 2.4 mmol/L and the 95% range should fall within the proposed limits of 2.2–2.6 mmol/L.
Secondly, as a further validation check, apply the equation prospectively to subsequent data sets (at least 250 calcium and albumin results collected using the same criteria).
The mean calculated adjusted calcium should be within 2× the standard error of the mean from the previous data; the 95% range should remain within the limits of 2.2–2.6.
Finally, the regression equation should be checked periodically (annually, or when any change of reagent or equipment occurs) using the same method. The slope and intercept of the new regression should remain within the 95% error limits output from the calculation of the original line. Any more significant change indicates a requirement to update the equation.
Assessment of response to the standardisation initiative
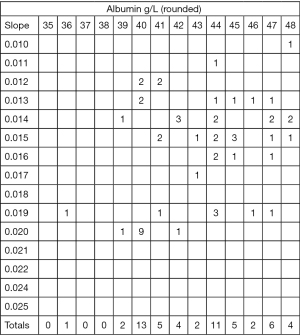
Following the initiatives described above, the expectation was that laboratories would move towards a more unified approach to calcium adjustment. At the very least, the use of locally derived adjustment equations should have been adopted, with few remaining laboratories using generic adjustment equations. In 2022, WEQAS conducted another survey of adjusted calcium equations currently in use (Figure 2). Comparison with Figure 1 shows a significant decrease in the proportion of labs using the equation of Payne et al.: 9/55 in comparison with 58/101 in the original surveys from 2008. In addition, 42 of the 55 respondents stated that their equation was locally derived.
Given the apparent significant increase in the use of locally derived equations the alignment of the equations to a mean adjusted calcium of 2.4 mmol/L as proposed by Pathology Harmony (or at least to the mean calcium of the local laboratory) should result in improved agreement around a consensus value for EQA samples compared with pre-2010 data. Even if many labs have not adopted the Pathology Harmony proposal improved accuracy and traceability of both calcium and albumin assays might be expected to improve inter-laboratory agreement
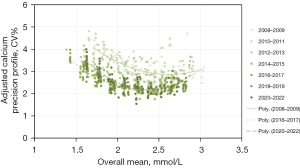
The WEQAS External Quality Assessment (EQA) Scheme has fortunately collected data over a long term which may be used to examine the response to the initiatives. Figure 3 shows the precision profile of all laboratory reports for adjusted calcium between 2008 and 2022. Samples with various calcium and albumin concentrations were distributed on multiple occasions annually and the adjusted calcium levels reported were compared with the consensus all-method mean. Examination of the curve shows a definite improvement in variation for the later data compared to 2008, but there is no evidence of further improvement since 2015.
Discussion
The essential purpose of calcium adjustment is to support clinicians when presented with an abnormal total calcium result by indicating whether the abnormality is primarily due to the patient's albumin concentration, or whether there is likely to be a disturbance of calcium metabolism which may require further investigation. The risk of the approach is that misclassification of patients as hyper- or hypocalcaemic due to a faulty adjustment equation may result in over-investigation or misdiagnosis. For this reason, there is value in the detailed examination of adjustment equations and exposure of various shortcomings and inaccuracies related to the proposed adjustment methods.
In a recent editorial (12), Weaving has summed up the current position with regard to calcium adjustment. He makes the pertinent point that forcing the data to fit a reference interval, either as originally proposed by Payne, to the mid-point of his laboratory reference interval, or as proposed by Pathology Harmony to a value of 2.4 mmol/L may not be scientifically sound, in particular if there is a proportionate bias in either calcium or albumin assays. Data from recent EQA reports, such as WEQAS, indicate that there are still examples of unacceptable systematic and proportional errors in both calcium and albumin assays (13). Any adjustment or standardisation is predicated on the assays supplying the data for the equation being fit for purpose. If assay EQA is persistently unacceptable then adjustment and standardisation will not perform well. In addition, there has been no UK audit of how adjustment equations are validated by individual laboratories, or how often. Failure to revalidate the equations following a change in reagent formulation or calibration material, for example, may result in sub-optimal performance.
Another issue which must be addressed is the derivation of the reference interval for adjusted calcium since this informs the classification of individuals as hyper, hypo- or normocalcaemic: essentially the aim of the adjustment exercise. Ideally, the reference interval for any adjustment equation should be derived by applying the total calcium and albumin results of a statistically significant cohort of individuals with no evidence of disordered calcium metabolism to the adjustment equation. Using the standardisation procedures described above the mean of the adjusted calcium range is set as 2.4 mmol/L; the reference interval is set pragmatically as 2.2–2.6 mmol/L, although examination of actual laboratory data may show a somewhat narrower range (14). It is important to emphasize that if a laboratory adjustment equation is set to a mean calcium significantly different from 2.4 mmol/L (or from the mean of the laboratory’s own reference range), then the use of 2.2–2.6 mmol/L (or the laboratory’s own reference range for total calcium) to classify patients’ calcium status will not be valid. A range specific to the adjustment equation should be derived in such cases.
An examination of recent literature shows that many authors persist in using published ‘correction’ equations from the literature—frequently that of Payne et al. (2) —as the basis for classification of patients’ calcium status (6,15-17). Unsurprisingly such classification performs poorly when compared with ionised calcium measurement, since without the use of locally generated adjustment equations the adjusted calcium data may be spurious (18). As a consequence, such comparative studies are unlikely to advance our understanding of the issue.
In terms of progress in the UK, the recent data from the WEQAS survey summarised in Figure 2 shows that a far higher proportion of laboratories are now using a locally derived equation compared to the data from 2008 (Figure 1). It should be noted that the data cannot be compared directly because there are fewer respondents in 2022 and the identity of the laboratories is not known. Despite this, there is a clear trend towards locally derived equations. This change may explain the improvement in inter-laboratory consensus for adjusted calcium EQA results as shown in Figure 3. However, other factors, such as improvements in performance and traceability of calcium and albumin assays may also be of relevance. Interestingly, the EQA data shows no further improvement since 2015. This may suggest that better consensus may not be possible given the state of the art of calcium and albumin assays. Proportionate biases in certain calcium methodologies (13) and inaccuracies at the lower limit of some albumin assays may introduce errors to the adjustment equations especially when using a single regression line (4). Further work is required on the data to determine whether bias or imprecision relating to certain assays is still a significant factor.
The approach to standardisation so far described makes assumptions regarding the physiology of calcium binding in vivo which are not reflected in sick patients. An adjustment which holds up reasonably for well patients may not be valid in such circumstances. Well documented examples include:
- Renal failure and other acute illnesses where acidosis alters the binding characteristics of calcium (19);
- Hypoalbuminaemia where both the accuracy of current albumin methods and the binding of calcium to other plasma proteins may distort the regression curve (4,20);
- Neonates where the binding characteristics may differ from those of adults (21).
Other rarer disorders which also affect binding have also been described (22).
As a means of countering the more common causes of inaccuracy the use of equations specific for certain disease groups (e.g., renal failure) have been proposed (23), but there is an issue of identifying patients for inclusion in a subgroup reliably. Also, if there are multiple equations, there is an increased administrative burden of validation and quality assurance. Another approach has been to include further parameters within the adjustment equation. Inclusion of phosphate (24) and blood pH (16,25) have been proposed. Even if such inclusions produce improvements in performance this benefit will need to be weighed against the cost of the additional testing required.
The alternative means to minimise misinterpretation is by education of clinicians of likely scenarios which distort adjustment, spotting outliers and including appropriate comments during result validation by senior scientific staff.
The effectiveness of whichever approach is adopted should be monitored through clinical audit.
The final problem in judging the success of a standard approach is the need to compare the outcome against a gold standard. The obvious candidate is ionised calcium especially since the assay is now available in most hospitals on POCT analysers. Comparative studies measuring total calcium, ionised calcium and PTH have shown that ionised calcium consistently outperforms total calcium for assessment of true physiological calcium status especially for investigation of primary hyperparathyroidism (26,27). The authors could find no studies in the literature comparing standardised adjusted calcium as described with ionised calcium and PTH levels. Such studies might provide a better understanding of those situations where laboratory calcium adjustment most often fails and the best ways to adopt some remedial action. If the shortcomings of the adjustment equations are better understood then there will be increased confidence in their use.
We are examining means of presenting calcium data to clinicians to achieve the best outcome for patients. Calcium adjustment equations appear to provide better information, but various shortcomings have questioned their utility in certain circumstances. Standardisation of adjustment is an attractive proposal with the aim of simplifying interpretation but the chemistries used for both calcium and albumin assays must be fit for purpose in order to achieve the standard approach—this may be through the Pathology Harmony route, or simply by the convergence of various assays and platforms to closer consensus and improved accuracy.
The physiological problems associated with calcium binding will need to be better appreciated, but there needs to be a balance between complexity of approach on the one hand and valid clinical output on the other. The increased use of ionised calcium is likely to become the preferred means of validating calcium status in situations where there is strong evidence that calcium adjustment formulae may produce unreliable results (28).
The strengths of this review are its ability for the first time to capture the development of calcium adjustment in the UK over a period of 50 years. It has described the major pitfalls of the process and also highlighted the importance of using valid cut-offs when making claims regarding the relative merits of actual calcium, adjusted calcium and ionised calcium for the assessment of physiological calcium status. Its main limitations have been the lack of sufficient EQA and audit data to back up claims of improvement in patient outcomes and better consensus in adjusted calcium reporting. Also, there is no published audit of ongoing validation of local adjustment equations. In addition, despite the extensive literature claiming the merits of various strategies of calcium reporting, the frequent inappropriate application of calcium adjustment has confounded many studies. This has limited the authors’ ability to make any definitive comments regarding best laboratory practice at present or in the near future.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Nuthar Jassam) for the series “Calcium Adjustment in Laboratory Medicine” published in Journal of Laboratory and Precision Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://jlpm.amegroups.com/article/view/10.21037/jlpm-22-35/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jlpm.amegroups.com/article/view/10.21037/jlpm-22-35/coif). The series “Calcium Adjustment in Laboratory Medicine” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Payne RB, Little AJ, Williams RB, et al. Interpretation of serum calcium in patients with abnormal serum proteins. Br Med J 1973;4:643-6. [Crossref] [PubMed]
- Payne RB, Carver ME, Morgan DB. Interpretation of serum total calcium: effects of adjustment for albumin concentration on frequency of abnormal values and on detection of change in the individual. J Clin Pathol 1979;32:56-60. [Crossref] [PubMed]
- Ashby JP, Wright DJ, Rinsler MG, et al. The adjusted serum calcium concept—a reappraisal. Ann Clin Biochem 1986;23:533-7. [Crossref] [PubMed]
- Barth JH, Fiddy JB, Payne RB. Adjustment of serum total calcium for albumin concentration: effects of non-linearity and of regression differences between laboratories. Ann Clin Biochem 1996;33:55-8. [Crossref] [PubMed]
- James MT, Zhang J, Lyon AW, et al. Derivation and internal validation of an equation for albumin-adjusted calcium. BMC Clin Pathol 2008;8:12. [Crossref] [PubMed]
- Gøransson LG, Skadberg Ø, Bergrem H. Albumin-corrected or ionized calcium in renal failure? What to measure? Nephrol Dial Transplant 2005;20:2126-9. [Crossref] [PubMed]
- Hill PG. The measurement of albumin in serum and plasma. Ann Clin Biochem 1985;22:565-78. [Crossref] [PubMed]
- Berg J. The Approach to Pathology Harmony in the UK. Clin Biochem Rev 2012;33:89-93. [PubMed]
- Berg J, Lane V. Pathology Harmony; a pragmatic and scientific approach to unfounded variation in the clinical laboratory. Ann Clin Biochem 2011;48:195-7. [Crossref] [PubMed]
- The Association of Clinical Biochemistry and Laboratory Medicine. Albumin-adjusted calcium: a position paper. March 2015. Available online: https://www.acb.org.uk/resource/adjusted-calcium-position-paper.html (Accessed 17 April, 2022).
- Jassam N, Hayden K, Dearman R, et al. Prospective study comparing the outcome of a population-specific adjusted calcium equation to ionized calcium. Ann Clin Biochem 2020;57:316-24. [Crossref] [PubMed]
- Weaving G. Calcium - An adjustment too far or not far enough? Ann Clin Biochem 2020;57:401-3. [Crossref] [PubMed]
- Jassam N, Thomas A, Hayden K, et al. The impact of the analytical performance specifications of calcium and albumin on adjusted calcium. Ann Clin Biochem 2020;57:382-8. [Crossref] [PubMed]
- Schini M, Hannan FM, Walsh JS, et al. Reference interval for albumin-adjusted calcium based on a large UK population. Clin Endocrinol (Oxf) 2021;94:34-9. [Crossref] [PubMed]
- Smith JD, Wilson S, Schneider HG. Misclassification of Calcium Status Based on Albumin-Adjusted Calcium: Studies in a Tertiary Hospital Setting. Clin Chem 2018;64:1713-22. [Crossref] [PubMed]
- Pekar JD, Grzych G, Durand G, et al. Calcium state estimation by total calcium: the evidence to end the never-ending story. Clin Chem Lab Med 2020;58:222-31. [Crossref] [PubMed]
- Yap E, Melaku Y, Puri I, et al. Predicting ionized hypocalcemia: External validation of an ionized calcium prediction model in patients with COVID-19 and renal failure. Ann Clin Biochem 2022;59:110-5. [Crossref] [PubMed]
- Scargill JJ, Guy JM. Validation of a locally derived serum calcium adjustment equation: relationship with total 25(OH) vitamin D and PTH levels. J Clin Pathol 2017;70:69-74. [Crossref] [PubMed]
- Wang S, McDonnell EH, Sedor FA, et al. pH effects on measurements of ionized calcium and ionized magnesium in blood. Arch Pathol Lab Med 2002;126:947-50. [Crossref] [PubMed]
- Sorva A. 'Correction' of serum calcium values for albumin biased in geriatric patients. Arch Gerontol Geriatr 1992;15:59-69. [Crossref] [PubMed]
- Jassam N, Gopaul S, McShane P, et al. Calcium adjustment equations in neonates and children. Ann Clin Biochem 2012;49:352-8. [Crossref] [PubMed]
- Walsh RL, Need AG, Coles ME. Albumin I.M.V.S.: a variant detected by a Bromcresol Green dye binding method. Clin Chim Acta 1983;130:11-23. [Crossref] [PubMed]
- Jain A, Bhayana S, Vlasschaert M, et al. A formula to predict corrected calcium in haemodialysis patients. Nephrol Dial Transplant 2008;23:2884-8. [Crossref] [PubMed]
- Ferrari P, Singer R, Agarwal A, et al. Serum phosphate is an important determinant of corrected serum calcium in end-stage kidney disease. Nephrology (Carlton) 2009;14:383-8. [Crossref] [PubMed]
- Kaku Y, Ookawara S, Miyazawa H, et al. New Method for the Approximation of Corrected Calcium Concentrations in Chronic Kidney Disease Patients. Ther Apher Dial 2016;20:46-52. [Crossref] [PubMed]
- Ong GS, Walsh JP, Stuckey BG, et al. The importance of measuring ionized calcium in characterizing calcium status and diagnosing primary hyperparathyroidism. J Clin Endocrinol Metab 2012;97:3138-45. [Crossref] [PubMed]
- Nordenström E, Katzman P, Bergenfelz A. Biochemical diagnosis of primary hyperparathyroidism: Analysis of the sensitivity of total and ionized calcium in combination with PTH. Clin Biochem 2011;44:849-52. [Crossref] [PubMed]
- Hamroun A, Pekar JD, Lionet A, et al. Ionized calcium: analytical challenges and clinical relevance. J Lab Precis Med 2020;5:22. [Crossref]
Cite this article as: Roberts G, Thomas A. Standardisation of adjusted calcium equation: the UK approach—a narrative review. J Lab Precis Med 2023;8:4.


