
The role of albumin level in cardiovascular disease: a review of recent research advances
Serum albumin
Serum albumin is an essential nutritional indicator, the major factor of oncotic pressure, and the modulator of body fluids (1). In clinical setting, serum albumin level is recognized as a simple and essential nutritional indicator and is generally used to evaluate the clinical courses of various diseases, including shock status, burns, bleeding event, trauma, hemorrhage, acute respiratory distress syndrome, terminal renal dysfunction, nutritional therapy, and post-resuscitation (2,3). Decrease in serum albumin level is common in critically ill patients and is mainly due to increased wasting, bleeding due to inflammation, and leakage of albumin from the gastrointestinal tract (1). Albumin level may also decrease as a result of redistribution from the intravascular space to the interstitial space due to increased capillary permeability, or as a reflection of poor nutritional status and liver function (4).
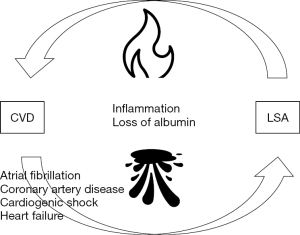
Regarding the action and pathophysiology of albumin, it is believed to have a significant relationship with cardiac dynamics and inflammation and has several characteristics in common with the aggravating factor of cardiovascular disease (CVD) (5). Thus, several studies have been conducted to clarify the relationship between serum albumin level and CVD.
In daily clinical setting, the serum albumin level under 3.5 g/dL is generally considered as hypoalbuminemia. However, there was no universal and clear definition of the low serum albumin (LSA) level to predict adverse events in cardiovascular medicine. Recent studies demonstrated an increased risk of cardiovascular events even at levels of 3.5–4.0 g/dL (6,7). In our previous study for patients admitted due to acute myocardial infarction (AMI), the serum albumin level under <3.8 g/dL was an independent predictor of adverse cardiac events at chronic phase of AMI (8). Therefore, we tentatively consider the serum albumin level under 3.8 g/dL as LSA of the risk factor in the area of cardiovascular medicine.
Previous reviews in 2010s have already summarized clinical evidence between serum albumin level and CVD (4). However, evidence including albumin level and bleeding event after CVD was not well taken in account. Furthermore, although serum albumin levels fluctuate depending on a patient’s general condition, the need and significance for reassessment during the chronic phase of CVD has not been sufficiently discussed.
In this review, we discuss the existing studies and recent evidence on the association between serum albumin level, especially LSA, and CVD and present future prospects for risk assessment of CVD, including coronary artery disease.
Serum albumin and CVD
Reports on serum albumin and CVD are extensive. LSA level has been reported to be associated with CVD, such as heart failure (HF), atrial fibrillation, and coronary artery disease (Figure 1).
Development of CVD
Several studies have indicated that LSA is an independent predictor of the development of HF (9,10). A registry study of 2,907 patients (9) and a large observational study of 5,795 health checkup patients who were followed up for 9.6 years demonstrated that LSA is an independent risk factor for the development of chronic HF. This result was consistent after adjusting for various inflammatory markers and body mass index (BMI) (10).
Several reports have been published regarding the association between albumin level and arrhythmia (11,12). Albumin level has been shown to be an independent prognostic factor for the development of atrial fibrillation, the most common arrhythmia in real-world clinical settings. In an observational study of 8,870 patients (8-year observation period) without CVD, LSA was a predictor of the development of atrial fibrillation in women. This result was independent of other cardiac diseases, BMI, and inflammatory markers (12). An observational study of 830 patients with CVD who underwent coronary artery bypass surgery showed the usefulness of serum albumin level in the development of postoperative atrial fibrillation (13).
Prognostic factors for CVD
LSA is considered a predictive factor for the development and prognosis of CVD. In addition, LSA has been reported to be a useful predictor of HF. In a study of 352 patients with chronic HF, LSA at initial presentation was associated with elevated N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels and increased long-term mortality (14). LSA has also been shown to be an independent predictor of short- and long-term events in patients with acute HF. A study of 546 patients with non-ischemic acute HF showed that LSA at admission is an independent predictor of adverse cardiac events (15). In these reports, the adverse effects of LSA were attributed to malnutrition, decrease in hepatic synthesis, elevated vascular permeability, and/or renal dysfunction. Other reports have linked albumin level to adverse outcomes in a wide range of CVDs, including venous thromboembolism (16,17).
In a study of 204 patients with chronic coronary syndrome conducted over a 708-day observation period, the results showed that LSA predicted adverse cardiac events, including all-cause mortality, stroke, and myocardial infarction (MI) (18). Furthermore, a study of 1,316 patients with chronic coronary syndrome and chronic kidney disease demonstrated that LSA at admission is a predictive factor for major adverse cardiac events (including all-cause mortality, stroke, and MI) in remote phase (19). These reports suggest that the primary cause of the negative effect of LSA is inflammation associated with severe atherogenesis.
Serum albumin and acute coronary syndrome (ACS)
Technological advances in primary reperfusion therapy, pharmacy, and physical therapy for ACS have reduced the incidence of short-term mortality in patients with ACS (20). The rate of in-hospital mortality among patients with ACS has improved as well, especially in the primary percutaneous coronary intervention (PCI) era (21). However, despite advances in multidisciplinary acute care for MI, the clinical need to manage the risks of HF and mortality, which are elevated in the remote phase of MI, remains unmet (22). Hence, risk stratification for the prevention of HF and mortality should be performed in the early phase of MI. Previous studies have shown that the following are important risk factors for HF and mortality in patients with MI: patient characteristic, electrocardiographic features, and factors of reperfusion therapy, ventricular function, and frailty status (23,24). Risk scores, such as the Global Registry of Acute Coronary Events (GRACE) score, have been established and are widely used (25,26). Albumin level is taken into account in some scores. Prognostic nutritional index is calculated using serum albumin and total lymphocyte count; geriatric nutritional risk index is calculated using serum albumin level and BMI; and controlling nutritional status score is calculated using the serum albumin level, total cholesterol, and total lymphocyte counts. These scores were also used as nutritional indicators and serve as significant prognostic factors in clinical outcomes in CVD (27-29). However, the clinical significance of albumin itself was not well identified in those existing models using multiple factors. Therefore, we examined the prognostic role of serum albumin level in CVD.
The prognostic impact of serum albumin level, a simple indicator, on cardiac events in the remote phase after ACS has been reported in several studies. A retrospective observational study of 7,192 patients with ACS showed that LSA (cutoff: 3.5 g/dL) at admission is an independent risk factor for in-hospital death and development of HF (6). There have also been several reports on hypoalbuminemia and the long-term prognosis of ACS (6,30). Our group conducted a single-center, retrospective observational study of 2,253 consecutive patients with AMI (8). In that study, the group with LSA (cutoff: 3.8 g/dL) in the acute phase of AMI showed a significantly increased frequency of adverse cardiac events (combined outcome of cardiovascular death and re-hospitalization for HF) in the chronic phase, indicating that LSA could be a prognostic factor for adverse cardiac events in patients with AMI. The results were consistent for each component of cardiovascular death and re-hospitalization for HF in the chronic phase of AMI, again demonstrating the clinical impact of risk stratification after AMI.
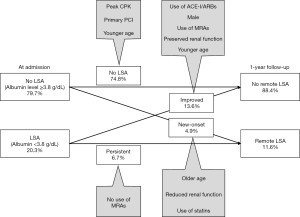
Regarding other adverse events, a single-center registry study demonstrated that LSA is useful for the risk stratification of bleeding events after PCI in patients with ACS, which is consistent with the results for the group without traditional bleeding risk factors (31). This finding was also reported in a multicenter registry study on AMI (32). In addition, a study of 1,724 consecutive patients with AMI undergoing PCI showed that LSA at admission is an independent predictor of chronic bleeding events. However, serum albumin levels are extremely variable during the acute phase of AMI owing to acute inflammation and circulatory dynamics (1). Some studies in which C-reactive protein/albumin ratio was used to account for the effects of inflammation showed its usefulness in predicting adverse cardiac events during hospitalization after coronary artery bypass surgery (33,34). Nevertheless, albumin levels may change with post-discharge medication use and change in nutritional intake status. Therefore, serum albumin levels measured in the acute phase of AMI alone may have limited predictive ability in the remote phase. The measurement of serum albumin levels during the chronic phase of AMI is expected to improve risk stratification. However, systematic reassessment in the chronic phase of AMI has not yet been fully established or implemented in real-world clinical settings. Hence, clinical evidence of the impact of such chronic transitions on post-MI prognosis is lacking. There are only a few studies on the association between chronic-phase serum albumin levels and long-term cardiovascular event. We conducted a single-center, retrospective, observational study of 1,424 consecutive patients with AMI to determine the changes in albumin levels from the acute phase of AMI to the chronic phase (one year later) in actual clinical practice (35). The results of the study suggest that LSA (cutoff: 3.8 g/dL) in the chronic phase of AMI, irrespective of the serum albumin level in the acute phase of AMI, is a predictive indicator for long-term outcomes in AMI patients. In particular, our report demonstrated that use of statins and renin-angiotensin-aldosterone system inhibitors at discharge might positively associated with serum albumin levels (Figure 2). Thus, albumin level measured in the chronic phase can be a prognostic indicator, even in patients who survive the acute phase of AMI. However, careful monitoring is needed, especially for AMI patients with remote LSA.
Pathophysiological speculation of serum albumin for adverse events
Effect of serum albumin on HF after ACS
Malnutrition status, decrease in hepatic synthesis, elevated vascular permeability, and frailty have been suggested as adverse effects of LSA on cardiovascular events. LSA may induce increased peripheral edematous and pulmonary congestion, even at lower left ventricular end systolic pressures, acting as an aggravating factor for HF (4). Such changes are likely to contribute to new onset of HF, particularly in patients with reduced cardiac function after ACS. Serum albumin level is widely known as a marker of inflammation. However, previous reports have shown an association between LSA status and left ventricular remodeling through the activation of cardiac inflammation (36). Furthermore, pathophysiological evaluation has shown that excessive inflammation contributes to left ventricular remodeling associated with new development of HF (37). The acute phase of ACS causes inflammation and temporarily decreases albumin levels (35). Inflammation and low albumin levels may have an additive negative impact on cardiovascular outcomes. Thus, further research on the association between inflammation and cardiac dysfunction is warranted.
Effect of serum albumin on bleeding events after ACS
Previous studies have indicated that the vulnerability of capillaries in systemic organs may be due to LSA (1). Protein metabolism plays an important role in tissue neogenesis and maintenance. Decreased albumin level is associated with tissue fragility, which consequently leads to fragility in vascular tissues and has a negative impact on bleeding events. Furthermore, LSA reflects malnutrition associated with vitamin C and K deficiencies. Vitamins C and K are essential for the coagulation system and play important roles in hemostasis during bleeding (38). Patients with LSA may simultaneously have vitamin deficiencies, which in turn may influence bleeding events after ACS. These multisystem factors may be responsible for increase in bleeding events after ACS in patients with LSA. However, the precise mechanism underlying high bleeding risk in patients with LSA is not well uncovered.
Limitation and future perspectives on the association between serum albumin and CVD
First, the detailed pathophysiological mechanisms underlying the serum albumin levels and adverse outcome are still uncertain. Future studies should be focused on albumin fluctuations from the acute to the chronic phase of CVD, because albumin fluctuations may help clarify the pathophysiology underlying the association between albumin level and CVD. Second, regarding the elevated albumin levels, there was little study examining the impact of non-LSA and elevated level of serum albumin levels in CVD. In an observational study for Korean, a higher serum albumin level was associated with an increased prevalence of metabolic syndrome (39). At the same time, an obesity paradox, in which overweight have a better prognosis compared with non-overweight/non-obese patients (40), is also well-known. Accordingly, there might be a possibility that an elevated level of serum albumin could play a protective role in cardiovascular medicine. In our recent study, among 289 AMI patients with LSA (<3.8 g/dL) at acute phase of AMI, 194 AMI patients (67.1%) showed improvement of albumin level (≥3.8 g/dL) at chronic phase. This improved subgroup demonstrated better outcomes in comparison with non-improved subgroup (35). However, it is still uncertain whether the higher the albumin levels, the better the prognosis in CVD. Third, evidence about the impact of interventions for increasing serum albumin levels on CVD is also uncovered. Albumin infusion therapy was significantly associated with a reduced risk of rebleeding and short-term mortality in patients with cirrhosis admitted for acute gastrointestinal bleeding (41). In contrast, recent retrospective observational study on the effect of albumin replacement in patients with HF did not show the significant clinical benefits of the therapy (42). Thus, the significance of interventions for LSA seems to remain controversial, which may partly result from differences in the methods of intervention and/or patient backgrounds, including disease status, among studies.
Serum albumin levels have been frequently used as a nutritional indicator. However, they could not reflect immediate changes in the nutritional and/or inflammatory statuses. Because prealbumin have shorter biologic half-life (2 days), compared with that of albumin (20 days), it would be sensitive to immediate changes in nutrition or inflammation (43). In a recent observational study, prealbumin was an independent factor to predict the development of HF after AMI (38). However, the clinical impact of prealbumin on cardiovascular events remains to be poorly understood. Association between prealbumin and serum albumin level, especially LSA, was also still unclear.
Conclusions
Serum albumin level has evolved as an indicator of nutrition and inflammation status, and its use in predicting the prognosis of CVD has recently been reported. Its usefulness in predicting bleeding events in coronary artery disease has also been reported, indicating its potential for comprehensive prediction of adverse events after ACS. Furthermore, evaluation of serum albumin levels in the chronic phase of ACS has shown the importance of risk stratification and post-ACS reassessment of LSA for the improvement of long-term prognosis. Further research on the pathophysiology of albumin level is needed to provide insight into the causal relationship between albumin levels and adverse events in CVD patients, which is currently unclear.
Acknowledgments
The authors thank Kensaku Nishihira, MD, and Yoshisato Shibata, MD (Miyazaki Medical Association Hospital, Miyazaki City, Japan) for their study support.
Funding: This work was supported by the Japan Society for the Promotion of Science (KAKENHI, Grant number: JP21K08130) and Takeda Science Foundation.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Tatsuo Shimosawa) for the series “New Biomarkers in Non-communicable Diseases” published in Journal of Laboratory and Precision Medicine. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jlpm.amegroups.com/article/view/10.21037/jlpm-22-57/coif). The series “New Biomarkers in Non-communicable Diseases” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fanali G, di Masi A, Trezza V, et al. Human serum albumin: from bench to bedside. Mol Aspects Med 2012;33:209-90. [Crossref] [PubMed]
- Cheng HC, Yang EH, Wu CT, et al. Hypoalbuminemia is a predictor of mortality and rebleeding in peptic ulcer bleeding under proton pump inhibitor use. J Formos Med Assoc 2018;117:316-25. [Crossref] [PubMed]
- Quero Alfonso AI, Fernández Castillo R, Fernández Gallegos R, et al. Study of serum albumin and BMI as nutritional markers in hemodialysis patients. Nutr Hosp 2014;31:1317-22. [PubMed]
- Arques S. Human serum albumin in cardiovascular diseases. Eur J Intern Med 2018;52:8-12. [Crossref] [PubMed]
- Arques S. Serum albumin and cardiovascular diseases: A comprehensive review of the literature. Ann Cardiol Angeiol (Paris) 2018;67:82-90. [Crossref] [PubMed]
- González-Pacheco H, Amezcua-Guerra LM, Sandoval J, et al. Prognostic Implications of Serum Albumin Levels in Patients With Acute Coronary Syndromes. Am J Cardiol 2017;119:951-8. [Crossref] [PubMed]
- Xia M, Zhang C, Gu J, et al. Impact of serum albumin levels on long-term all-cause, cardiovascular, and cardiac mortality in patients with first-onset acute myocardial infarction. Clin Chim Acta 2018;477:89-93. [Crossref] [PubMed]
- Yoshioka G, Tanaka A, Nishihira K, et al. Prognostic Impact of Serum Albumin for Developing Heart Failure Remotely after Acute Myocardial Infarction. Nutrients 2020;12:2637. [Crossref] [PubMed]
- Gopal DM, Kalogeropoulos AP, Georgiopoulou VV, et al. Serum albumin concentration and heart failure risk The Health, Aging, and Body Composition Study. Am Heart J 2010;160:279-85. [Crossref] [PubMed]
- Filippatos GS, Desai RV, Ahmed MI, et al. Hypoalbuminaemia and incident heart failure in older adults. Eur J Heart Fail 2011;13:1078-86. [Crossref] [PubMed]
- Wang Y, Du P, Xiao Q, et al. Relationship Between Serum Albumin and Risk of Atrial Fibrillation: A Dose-Response Meta-Analysis. Front Nutr 2021;8:728353. [Crossref] [PubMed]
- Mukamal KJ, Tolstrup JS, Friberg J, et al. Fibrinogen and albumin levels and risk of atrial fibrillation in men and women (the Copenhagen City Heart Study). Am J Cardiol 2006;98:75-81. [Crossref] [PubMed]
- Karabacak K, Kubat E, Akyol FB, et al. The C-reactive protein/albumin ratio as a new predictor for postoperative atrial fibrillation after coronary artery bypass graft surgery. J Card Surg 2020;35:2747-53. [Crossref] [PubMed]
- Yi S, Chen M. Decreased albumin is associated with elevated N-terminal pro-brain natriuretic peptide and poor long-term prognosis in patients with chronic heart failure. Medicine (Baltimore) 2020;99:e23872. [Crossref] [PubMed]
- Ancion A, Allepaerts S, Oury C, et al. Serum albumin level and hospital mortality in acute non-ischemic heart failure. ESC Heart Fail 2017;4:138-45. [Crossref] [PubMed]
- Folsom AR, Lutsey PL, Heckbert SR, et al. Serum albumin and risk of venous thromboembolism. Thromb Haemost 2010;104:100-4. [Crossref] [PubMed]
- Königsbrügge O, Posch F, Riedl J, et al. Association Between Decreased Serum Albumin With Risk of Venous Thromboembolism and Mortality in Cancer Patients. Oncologist 2016;21:252-7. [Crossref] [PubMed]
- Suzuki S, Hashizume N, Kanzaki Y, et al. Prognostic significance of serum albumin in patients with stable coronary artery disease treated by percutaneous coronary intervention. PLoS One 2019;14:e0219044. [Crossref] [PubMed]
- Wada H, Dohi T, Miyauchi K, et al. Long-term clinical impact of serum albumin in coronary artery disease patients with preserved renal function. Nutr Metab Cardiovasc Dis 2018;28:285-90. [Crossref] [PubMed]
- Decramer M, Devos P, De Roo M, et al. Evaluation of bedside myocardial scintigraphy with 201Tl in acute myocardial infarction. Eur J Nucl Med 1982;7:200-3. [Crossref] [PubMed]
- Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 2000;283:2941-7. [Crossref] [PubMed]
- O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 2013;82:E1-27. [Crossref] [PubMed]
- Shimizu A. What are the most useful predictors of cardiac mortality in patients post myocardial infarction? Circ J 2013;77:319-20. [Crossref] [PubMed]
- Nishihira K, Yoshioka G, Kuriyama N, et al. Impact of frailty on outcomes in elderly patients with acute myocardial infarction who undergo percutaneous coronary intervention. Eur Heart J Qual Care Clin Outcomes 2021;7:189-97. [Crossref] [PubMed]
- D'Ascenzo F, Biondi-Zoccai G, Moretti C, et al. TIMI, GRACE and alternative risk scores in Acute Coronary Syndromes: a meta-analysis of 40 derivation studies on 216,552 patients and of 42 validation studies on 31,625 patients. Contemp Clin Trials 2012;33:507-14. [Crossref] [PubMed]
- Goriki Y, Tanaka A, Yoshioka G, et al. Development of a Laboratory Risk-Score Model to Predict One-Year Mortality in Acute Myocardial Infarction Survivors. J Clin Med 2022;11:3497. [Crossref] [PubMed]
- Cheng YL, Sung SH, Cheng HM, et al. Prognostic Nutritional Index and the Risk of Mortality in Patients With Acute Heart Failure. J Am Heart Assoc 2017;6:e004876. [Crossref] [PubMed]
- Yoo SH, Kook HY, Hong YJ, et al. Influence of undernutrition at admission on clinical outcomes in patients with acute myocardial infarction. J Cardiol 2017;69:555-60. [Crossref] [PubMed]
- Basta G, Chatzianagnostou K, Paradossi U, et al. The prognostic impact of objective nutritional indices in elderly patients with ST-elevation myocardial infarction undergoing primary coronary intervention. Int J Cardiol 2016;221:987-92. [Crossref] [PubMed]
- He YM, Yang Q, Yang XJ, et al. Serum albumin concentrations, effect modifiers and first incident acute myocardial infarction: A cross-sectional study of 1552 cases and 6680 controls. Clin Chim Acta 2016;454:49-56. [Crossref] [PubMed]
- Tatami Y, Ishii H, Aoki T, et al. Decreased Serum Albumin Predicts Bleeding Events in Patients on Antiplatelet Therapy After Percutaneous Coronary Intervention. Circ J 2017;81:999-1005. [Crossref] [PubMed]
- Yoshioka G, Natsuaki M, Goriki Y, et al. Serum Albumin and Bleeding Events After Percutaneous Coronary Intervention in Patients With Acute Myocardial Infarction (from the HAGAKURE-ACS Registry). Am J Cardiol 2022;165:19-26. [Crossref] [PubMed]
- Aksoy F, Uysal D, Ibrişim E. Relationship between c-reactive protein/albumin ratio and new-onset atrial fibrillation after coronary artery bypass grafting. Rev Assoc Med Bras (1992) 2000;66:1070-6. [PubMed]
- Aksoy F, Uysal D, Ibrişim E. Predictive values of C-reactive protein/albumin ratio in new-onset atrial fibrillation after coronary artery bypass grafting. Rev Assoc Med Bras (1992) 2000;66:1049-56. [PubMed]
- Yoshioka G, Tanaka A, Nishihira K, et al. Prognostic impact of follow-up serum albumin after acute myocardial infarction. ESC Heart Fail 2021;8:5456-65. [Crossref] [PubMed]
- Mann DL. Innate immunity and the failing heart: the cytokine hypothesis revisited. Circ Res 2015;116:1254-68. [Crossref] [PubMed]
- Westman PC, Lipinski MJ, Luger D, et al. Inflammation as a Driver of Adverse Left Ventricular Remodeling After Acute Myocardial Infarction. J Am Coll Cardiol 2016;67:2050-60. [Crossref] [PubMed]
- Kawai M, Harada M, Motoike Y, et al. Impact of serum albumin levels on supratherapeutic PT-INR control and bleeding risk in atrial fibrillation patients on warfarin: A prospective cohort study. Int J Cardiol Heart Vasc 2019;22:111-6. [Crossref] [PubMed]
- Cho HM, Kim HC, Lee JM, et al. The association between serum albumin levels and metabolic syndrome in a rural population of Korea. J Prev Med Public Health 2012;45:98-104. [Crossref] [PubMed]
- Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol 2009;53:1925-32. [Crossref] [PubMed]
- Wang Z, Xie YW, Lu Q, et al. The impact of albumin infusion on the risk of rebleeding and in-hospital mortality in cirrhotic patients admitted for acute gastrointestinal bleeding: a retrospective study of a single institute. BMC Gastroenterol 2020;20:198. [Crossref] [PubMed]
- Wang L, Zhao YT. Albumin infusion in hospitalized patients with acute heart failure: a retrospective cohort study. BMC Cardiovasc Disord 2022;22:358. [Crossref] [PubMed]
- Beck FK, Rosenthal TC. Prealbumin: a marker for nutritional evaluation. Am Fam Physician 2002;65:1575-8. [PubMed]
Cite this article as: Yoshioka G, Tanaka A, Goriki Y, Node K. The role of albumin level in cardiovascular disease: a review of recent research advances. J Lab Precis Med 2023;8:7.


